Trendelenburg Test
content of this page
1- Introduction
2- Anatomical Overview
3- Causes
4- Treatment
Introduction
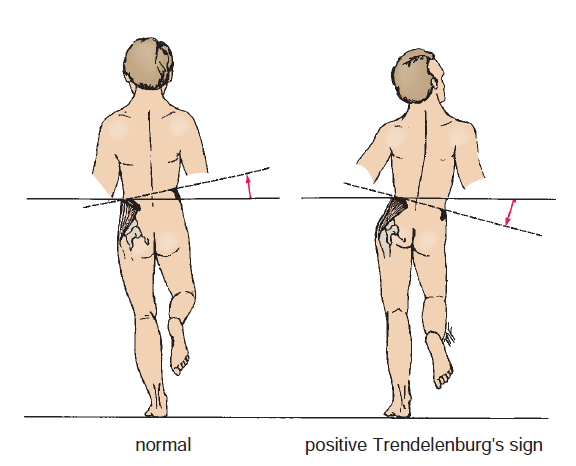
The Trendelenburg test of the hip is a physical examination maneuver used to assess the strength and function of the hip abductor muscles, particularly the gluteus medius. During the test, the patient stands on one leg while the healthcare provider observes the position of the pelvis. If the pelvis drops on the unsupported side, it may indicate weakness or dysfunction of the hip abductor muscles on the weight-bearing side. This test is commonly used to evaluate hip stability and can help diagnose conditions such as hip abductor muscle weakness or hip joint problems.
Anatomical Overview
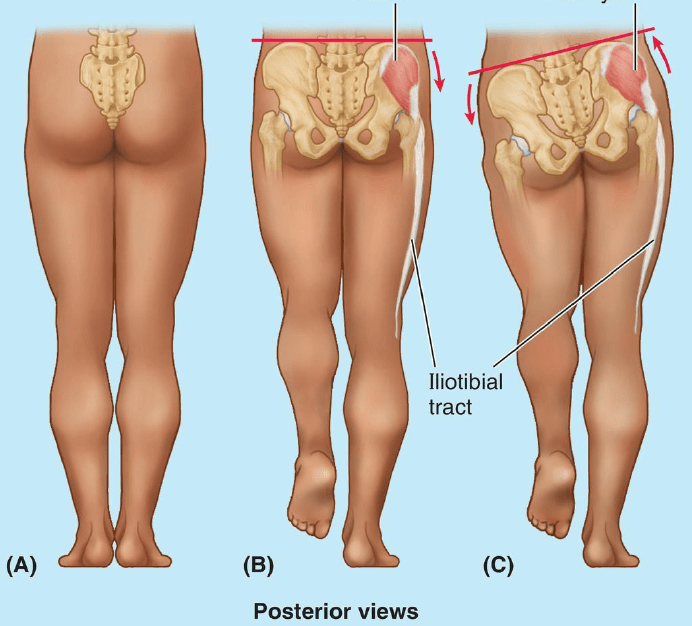
The hip joint, a ball-and-socket joint, connects the thigh bone (femur) to the pelvis. It is stabilized by a group of muscles, including the gluteus medius, which plays a crucial role in hip abduction. The gluteus medius muscle originates from the outer surface of the ilium, specifically the iliac crest and the area just below it known as the gluteal aponeurosis. From there, it runs obliquely downward and laterally to insert into the greater trochanter of the femur. This muscle is responsible for various movements, including abduction (moving the leg away from the midline of the body), internal rotation, and stabilization of the pelvis during activities such as walking or running.
The Trendelenburg test specifically targets the function of the gluteus medius muscle. During the test, the patient stands on one leg, which activates the hip abductor muscles to stabilize the pelvis. The healthcare provider observes the position of the pelvis from behind. If the pelvis drops on the unsupported side (the side opposite to the weight-bearing leg), it indicates that the hip abductor muscles, including the gluteus medius, on the weight-bearing side are weak or dysfunctional. This drop in the pelvis is a positive Trendelenburg sign and can be indicative of various conditions affecting the hip joint, such as hip abductor muscle weakness, hip arthritis, or hip joint instability.
Causes
Hip Abductor Muscle Weakness: This is the most common cause. Weakness of the gluteus medius muscle, often due to injury, disuse, or neurological conditions, can lead to a positive Trendelenburg sign.
Hip Joint Pathology: Conditions affecting the hip joint, such as arthritis, hip dysplasia, or a labral tear, can result in hip joint instability and a positive Trendelenburg sign.
Nerve Damage: Damage to the superior gluteal nerve, which innervates the gluteus medius muscle, can lead to muscle weakness and a positive Trendelenburg sign. This can occur due to conditions such as diabetic neuropathy or nerve injury during surgery.
Spinal Conditions: Spinal disorders affecting the nerve roots that supply the gluteus medius muscle, such as lumbar disc herniation or spinal stenosis, can result in weakness and a positive Trendelenburg sign.
Musculoskeletal Imbalance: Imbalance between the hip abductor muscles and the hip adductor muscles can lead to a positive Trendelenburg sign. This can occur due to overuse or underuse of these muscle groups.
Congenital Abnormalities: Rarely, congenital abnormalities affecting the development of the hip joint or its supporting structures can result in hip instability and a positive Trendelenburg sign.
Treatment
Physical Therapy: Physical therapy can help strengthen the hip abductor muscles, improve hip joint stability, and correct gait abnormalities. Exercises may focus on strengthening the gluteus medius and other hip abductor muscles.
Activity Modification: Avoiding activities that worsen the Trendelenburg sign, such as prolonged standing or walking, may be recommended.
Assistive Devices: In some cases, using assistive devices such as a cane or walker can help improve stability and reduce the risk of falling.
Orthotics: Custom orthotic devices, such as shoe inserts, can help correct foot alignment and improve gait mechanics, which may alleviate symptoms.
Surgery: In cases where the Trendelenburg sign is caused by structural abnormalities or severe muscle weakness that does not respond to conservative treatment, surgery may be considered. Surgical options may include hip joint repair, muscle tendon transfer, or joint replacement.
Medication: In some cases, medications such as nonsteroidal anti-inflammatory drugs (NSAIDs) may be prescribed to help reduce pain and inflammation associated with hip joint pathology.