Heart Failure
Content of This Page
1- Introduction
2- Causes
3– Pathophysiology
4- Signs & Symptoms
5- Types
6- Investigations & Lab Results
7- Complications
8- Treatment
Introduction
Heart failure is a clinical syndrome characterized by the heart’s inability to pump blood adequately to meet the body’s metabolic needs. It results from structural or functional cardiac disorders that impair the ability of the ventricles to fill with or eject blood effectively. This condition can be classified based on the ejection fraction into heart failure with reduced ejection fraction (HFrEF), heart failure with preserved ejection fraction (HFpEF), and heart failure with mildly reduced ejection fraction (HFmrEF).Heart failure may be acute, with sudden onset of symptoms, or chronic, developing gradually over time
Causes
-Heart failure can be caused by a range of conditions and factors, including:
Coronary Artery Disease (CAD): Blockages in the heart’s arteries reduce blood flow to the heart muscle, leading to damage and decreased pumping efficiency.
High Blood Pressure (Hypertension): Elevated blood pressure forces the heart to work harder, which can weaken the heart over time.
Heart Attack (Myocardial Infarction): Damage from a heart attack can impair the heart’s ability to pump effectively.
Cardiomyopathy: Diseases of the heart muscle, which can be caused by various factors including infections, alcohol abuse, or genetic conditions.
Valvular Heart Disease: Problems with the heart’s valves (e.g., stenosis or regurgitation) can affect blood flow and lead to heart failure.
Arrhythmias: Irregular heartbeats can disrupt the heart’s ability to pump blood efficiently.
Congenital Heart Defects: Structural issues present at birth can contribute to heart failure.
Diabetes: Diabetes can damage blood vessels and nerves that control the heart, leading to heart failure.
Chronic Lung Diseases: Conditions like chronic obstructive pulmonary disease (COPD) can strain the heart and contribute to heart failure.
Other Factors: Severe anemia, thyroid disorders, and certain infections can also impact heart function and lead to heart failure.
Pathophysiology
- Decreased Cardiac Output → Activation of Sympathetic Nervous System
↓ Cardiac output leads to ↓ blood pressure, triggering increased sympathetic activity. This causes vasoconstriction and increased heart rate and contractility. While initially helpful, chronic sympathetic stimulation leads to increased myocardial oxygen demand, arrhythmias, and ventricular remodeling. - Activation of the Renin-Angiotensin-Aldosterone System (RAAS)
↓ Renal perfusion activates RAAS → leads to vasoconstriction (via angiotensin II) and sodium and water retention (via aldosterone). This increases preload and afterload, further straining the heart. - Release of Antidiuretic Hormone (ADH)
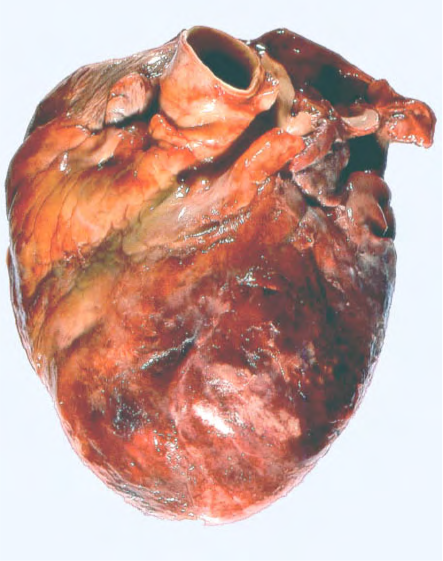
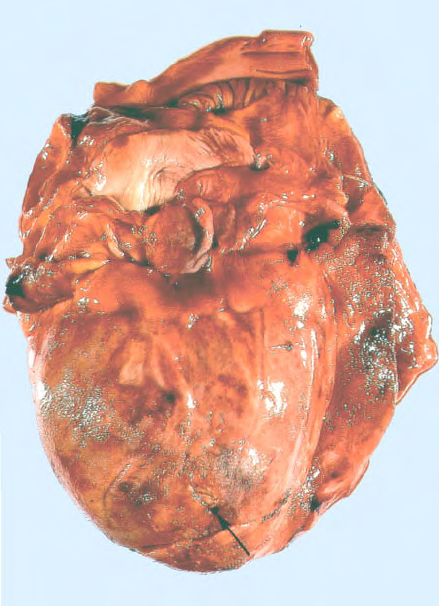
ADH promotes water reabsorption from the kidneys, contributing to fluid overload and worsening edema. - Ventricular Remodeling and Hypertrophy
Chronic pressure and volume overload result in structural changes in the heart, including hypertrophy and dilation. These changes reduce contractility and contribute to the progression of heart failure. - Natriuretic Peptide Response
As a compensatory mechanism, the heart releases B-type natriuretic peptide (BNP) and atrial natriuretic peptide (ANP), which promote vasodilation and diuresis. However, their effects are often overwhelmed by the stronger vasoconstrictive and fluid-retaining mechanisms.
Signs & Symptoms
-General Symptoms (due to low cardiac output):
Fatigue
Weakness
Exercise intolerance
Cold extremities
Dizziness or confusion (in severe cases)
-Left-Sided Heart Failure:
Pulmonary congestion symptoms:
Dyspnea on exertion
Orthopnea (shortness of breath when lying flat)
Paroxysmal nocturnal dyspnea (sudden nighttime breathlessness)
Cough (often worse at night)
Nocturnal wheezing
Pulmonary crackles on auscultation
Cyanosis in advanced cases
-Right-Sided Heart Failure:
Systemic venous congestion symptoms:
Peripheral edema (especially in ankles and legs)
Jugular venous distension (JVD)
Hepatomegaly (enlarged liver)
Ascites (fluid in the abdomen)
Right upper quadrant discomfort or pain
Weight gain due to fluid retention
-Other Signs on Physical Examination:
Tachycardia
Hypotension (in advanced stages)
Displaced apex beat
Third heart sound (S3) in systolic heart failure
Cool, clammy skin in cardiogenic shock
Pulsus alternans (alternating strong and weak pulses)

Types
1. Based on Ejection Fraction (EF):
Heart Failure with Reduced Ejection Fraction (HFrEF):
EF less than 40%
Also called systolic heart failure
Characterized by impaired ventricular contraction and reduced cardiac output
Heart Failure with Preserved Ejection Fraction (HFpEF):
EF 50% or greater
Also called diastolic heart failure
Characterized by impaired ventricular relaxation and filling, despite normal contractility
Heart Failure with Mid-Range or Mildly Reduced Ejection Fraction (HFmrEF):
EF between 41% and 49%
Represents an intermediate group with features of both systolic and diastolic dysfunction
2. Based on Side of the Heart Affected:
Left-Sided Heart Failure:
Most common type
Leads to pulmonary congestion and symptoms related to poor oxygenation
Right-Sided Heart Failure:
Often occurs secondary to left-sided failure or lung disease (cor pulmonale)
Leads to systemic venous congestion and fluid retention
Biventricular Failure:
Both right and left ventricles are involved
Presents with combined symptoms of both sides
3. Based on Onset and Course:
Acute Heart Failure:
Sudden onset or worsening of symptoms
Often due to myocardial infarction, arrhythmia, or acute valve dysfunction
Chronic Heart Failure:
Gradual development and progression of symptoms
Usually due to chronic conditions like hypertension or cardiomyopathy
Investigations & Lab Results
1. Laboratory Tests:
B-type Natriuretic Peptide (BNP) and N-terminal pro-BNP (NT-proBNP):
Elevated levels support the diagnosis of heart failure
Levels correlate with severity and prognosis
Can help differentiate cardiac from non-cardiac causes of dyspnea
Complete Blood Count (CBC):
To check for anemia or infection which may worsen HF symptoms
Serum Electrolytes:
Sodium, potassium, calcium, and magnesium
Important for monitoring diuretic therapy and detecting electrolyte imbalances
Renal Function Tests (Blood Urea Nitrogen and Creatinine):
Assess kidney function, which may be impaired due to reduced perfusion or medications
Liver Function Tests:
May be elevated due to hepatic congestion in right-sided failure
Thyroid Function Tests:
Hyperthyroidism or hypothyroidism can precipitate or worsen heart failure
Cardiac Enzymes (Troponin):
To rule out acute myocardial infarction as a cause of acute heart failure
2. Electrocardiogram (ECG):
May show evidence of ischemia, previous myocardial infarction, arrhythmias, left ventricular hypertrophy, or conduction abnormalities
3. Chest X-ray:
Signs of pulmonary congestion:
Cardiomegaly (enlarged heart silhouette)
Pulmonary venous congestion
Interstitial edema or alveolar edema (bat-wing pattern)
Pleural effusions
4. Echocardiography:
Essential for diagnosis and classification
Assesses ejection fraction, ventricular size and function
Identifies valvular abnormalities, pericardial disease, and wall motion abnormalities
Guides treatment decisions
5. Other Imaging:
Cardiac MRI: Detailed assessment of myocardial structure and function
Coronary Angiography: If ischemic heart disease is suspected as the cause
Stress Testing: To evaluate ischemia and exercise tolerance
Complications
Cardiogenic shock
Arrhythmias (e.g., atrial fibrillation, ventricular tachycardia)
Thromboembolism
Renal dysfunction
Hepatic congestion and cirrhosis
Pulmonary hypertension
Cachexia and muscle wasting
Sudden cardiac death
Treatment
ACE Inhibitors (or ARBs if ACE inhibitors are not tolerated):
Reduce mortality and morbidity by blocking the renin-angiotensin system
Examples: enalapril, lisinopril, ramipril
Diuretics:
Used to relieve symptoms of fluid overload such as edema and pulmonary congestion
Examples: furosemide, hydrochlorothiazide
Improve symptoms but do not reduce mortality
Beta-Blockers:
Reduce sympathetic overactivity, improve survival and reduce hospitalizations
Examples: bisoprolol, carvedilol, metoprolol succinate
Mineralocorticoid Receptor Antagonists (MRAs):
Reduce fluid retention and improve outcomes
Examples: spironolactone, eplerenone
SGLT2 Inhibitors:
Shown to reduce hospitalization and mortality in heart failure
Examples: dapagliflozin, empagliflozin
Other Medications:
Angiotensin Receptor-Neprilysin Inhibitor (ARNI):
Combination of sacubitril and valsartan, superior to ACE inhibitors in some cases
Ivabradine:
Used to reduce heart rate in patients with high resting heart rate despite beta-blocker therapy
Digoxin:
Limited use for symptom control and rate control in atrial fibrillation