Alcoholic Liver Disease (ALD)
Content of This Page
1- Introduction
2- Pathophysiology
3- Symptoms
4- Stages of The Disease
5- Treatment
6- What Should You Avoid
Introduction
Alcoholic Liver Disease (ALD) refers to a range of liver conditions caused by chronic and excessive alcohol consumption. It represents a major cause of chronic liver disease globally and contributes significantly to liver-related morbidity and mortality. The disease spectrum includes:
Alcohol-related fatty liver (steatosis)
Alcoholic hepatitis
Alcoholic cirrhosis
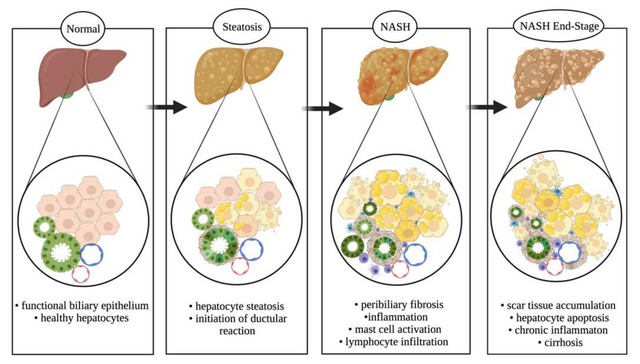
Pathophysiology
1-Ethanol metabolism in the liver generates acetaldehyde and reactive oxygen species (ROS).These damage hepatocytes by disrupting proteins, lipids, and DNA.
2-Fatty liver (steatosis) develops as alcohol:
- Inhibits fat breakdown (β-oxidation) and promotes fat synthesis.
- Causes triglyceride accumulation in hepatocytes.
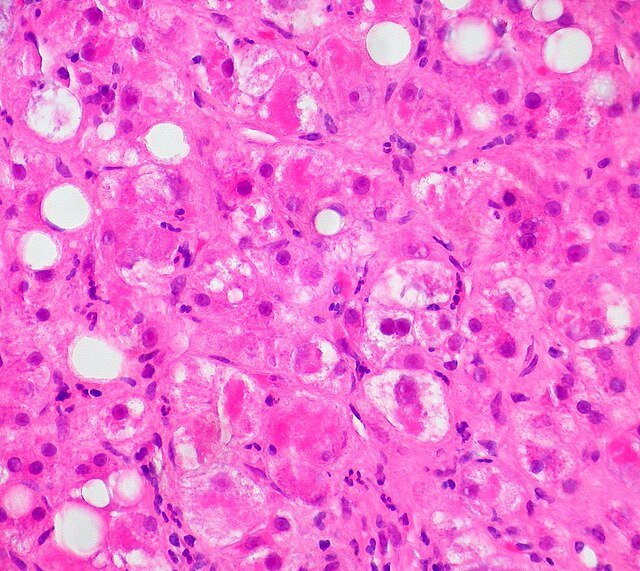
3-Alcoholic hepatitis arises from:
-
Inflammatory cytokines (e.g. TNF-α) and immune cell infiltration.
-
Hepatocyte ballooning and formation of Mallory-Denk bodies.
4-Fibrosis and cirrhosis result from:
- Activation of hepatic stellate cells → collagen deposition.
- Architectural distortion of the liver with loss of function.
5-Modifying factors include:
- Genetics (e.g. PNPLA3 variants), obesity, viral hepatitis, and malnutrition.
Symptoms
Fatty Liver:
Often asymptomatic
May have fatigue or mild right upper abdominal discomfort
Alcoholic Hepatitis:
Jaundice, fever, nausea, RUQ pain
Anorexia, weight loss, fatigue
Severe cases: confusion (encephalopathy), bleeding, renal issues
Alcoholic Cirrhosis:
Abdominal swelling (ascites), leg oedema
Vomiting blood (variceal bleeding), confusion
Hormonal signs: spider naevi, gynaecomastia, testicular atrophy
Chronic signs: muscle wasting, Dupuytren’s contracture, parotid swelling
Stages of The Disease
1-Fatty Liver (Steatosis):
- Fat builds up in liver cells
- Usually silent and fully reversible with alcohol abstinence
2-Alcoholic Hepatitis:
- Inflammatory liver injury with jaundice, fever, and RUQ pain
- Can be severe and life-threatening, but partially reversible
3-Alcoholic Cirrhosis:
- Permanent liver scarring and dysfunction
- Features: ascites, encephalopathy, bleeding
- Irreversible, but abstinence may slow progression
Treatment
1-Alcohol Abstinence:
- Most important intervention
- Improves outcomes at all stages
- Requires counselling and rehabilitation support
2-Nutritional Support:
- High-protein, high-calorie diet
- Supplement vitamins (e.g. thiamine, folate, zinc)
3-Alcoholic Hepatitis (Severe Cases):
- Corticosteroids (e.g. prednisolone) if DF >32
- N-acetylcysteine (NAC) may be added
- Stop steroids if no response at 7 days
4-Cirrhosis Management:
- Standard treatment for ascites, varices, and encephalopathy
- Monitor for complications
5-Liver Transplantation:
- Consider in end-stage disease
- Requires sustained abstinence and psychosocial assessment
What Should You Avoid
1-Alcohol – Absolute avoidance is essential at all stages.
2-Liver-toxic drugs – Avoid high-dose paracetamol, NSAIDs, and certain antibiotics.
3-Sedatives (e.g. benzodiazepines) – Can worsen hepatic encephalopathy.
4-High-salt diet – Exacerbates ascites and oedema.
5-Herbal or unregulated supplements – May be toxic to the liver.
6-Smoking – Accelerates liver damage and fibrosis.
7-Raw shellfish or contaminated food – Increases infection risk in cirrhotic patients.