Gastroesophageal Reflux Disease
content of this page
1- Introduction
2- Pathophysiology
3- Symptoms
4- Treatment
Introduction
Gastroesophageal Reflux Disease (GERD) is a chronic digestive disorder where stomach acid or bile irritates the food pipe lining. This often causes heartburn, a burning sensation in the chest, and can lead to other symptoms like regurgitation, difficulty swallowing, and chronic cough. GERD can impact daily life and may require management through lifestyle changes, medications, or in severe cases, surgery.
Pathophysiology
Gastroesophageal Reflux Disease (GERD) is characterized by the chronic backflow of stomach contents, including acid and bile, into the esophagus due to dysfunction of the lower esophageal sphincter (LES) and other contributing factors. Normally, the LES acts as a valve that opens to allow food and liquids into the stomach and closes to prevent reflux. In GERD, this valve mechanism is compromised, often due to factors such as obesity, hiatal hernia, or medications that relax the LES. This allows stomach acid to irritate the esophageal lining, leading to symptoms such as heartburn, regurgitation, and difficulty swallowing. Prolonged exposure to gastric contents can cause inflammation and erosion of the esophageal mucosa, resulting in complications like erosive esophagitis and, in severe cases, Barrett’s esophagus or esophageal cancer.

Symptoms
Heartburn: A burning sensation in the chest that often occurs after eating or at night, particularly when lying down.
Regurgitation: The sensation of acid or food backing up into the throat or mouth, often accompanied by a sour or bitter taste.
Dysphagia: Difficulty swallowing, which may feel like food is sticking in the throat or chest.
Chest Pain: Some individuals may experience chest pain that can mimic the symptoms of a heart attack, especially when GERD is severe or untreated.
Chronic Cough: A persistent cough, often worse at night, that may be due to irritation of the throat and airways from acid reflux.
Hoarseness or Sore Throat: Irritation of the vocal cords or throat due to acid reflux, leading to changes in voice quality or persistent soreness.
Worsening Asthma Symptoms: Acid reflux can aggravate asthma symptoms, particularly coughing and wheezing.
Feeling of a Lump in the Throat: Sensation of a lump or tightness in the throat, known as globus sensation, which may be related to acid irritation.
Dental Erosion: Acidic reflux can contribute to tooth enamel erosion and dental problems over time.
Treatment
1. Lifestyle Modifications:
- Dietary Changes: Avoiding trigger foods that can worsen symptoms, such as spicy or acidic foods, caffeine, chocolate, and fatty foods. Adopting a low-fat diet and smaller, more frequent meals can also help.
- Weight Management: Losing weight, if overweight or obese, can reduce pressure on the abdomen and lower the risk of reflux.
- Elevating the Head of the Bed: Raising the head of the bed by 6 to 8 inches can help prevent nighttime reflux.
- Avoiding Tight Clothing: Looser clothing around the abdomen can reduce pressure on the stomach and LES.
- Smoking Cessation: Quitting smoking can improve LES function and reduce reflux symptoms.
2. Medications:
- Proton Pump Inhibitors (PPIs): These medications reduce stomach acid production and are highly effective in treating GERD symptoms and healing esophageal damage. Examples include omeprazole (Prilosec), esomeprazole (Nexium), and lansoprazole (Prevacid).
- H2 Blockers: Histamine-2 receptor antagonists, such as ranitidine (Zantac) and famotidine (Pepcid), reduce acid production and can be used as an alternative to PPIs or in combination therapy.
- Antacids: Over-the-counter antacids like Tums or Maalox provide quick relief by neutralizing stomach acid. They are often used for milder symptoms or as adjunct therapy.
3. Surgical Interventions:
- Fundoplication: A surgical procedure where the upper part of the stomach is wrapped around the LES to strengthen it and prevent reflux.
- LINX Device: A minimally invasive procedure where a magnetic ring is placed around the LES to help it stay closed when not swallowing.
4. Monitoring and Follow-Up:
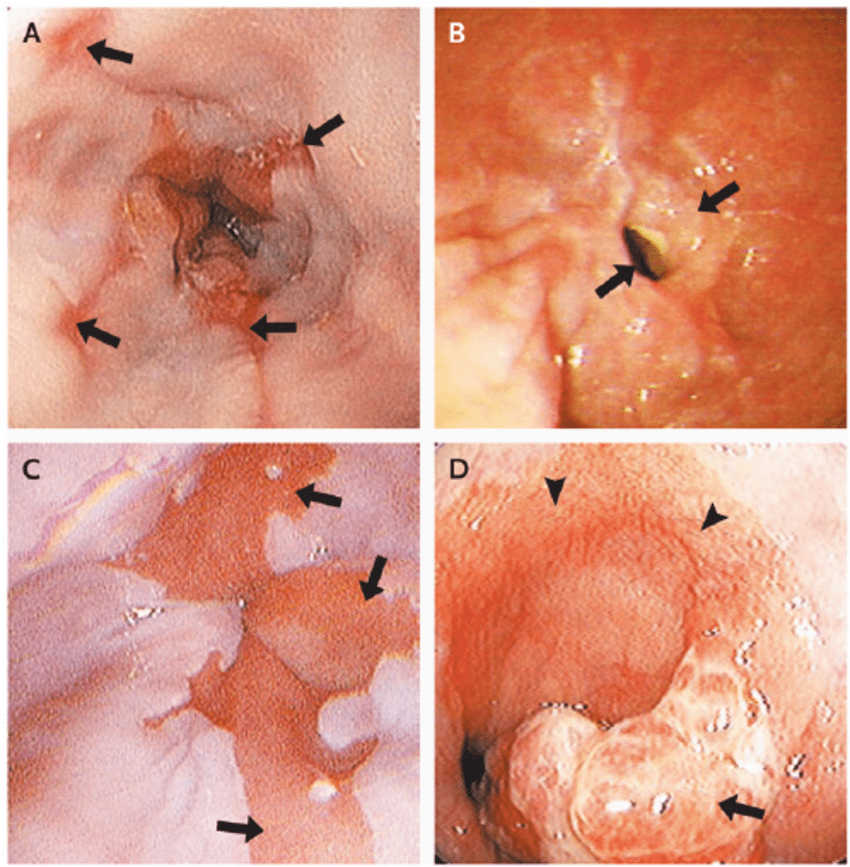
- Endoscopy: For individuals with severe symptoms or complications, an endoscopy may be recommended to assess the extent of esophageal damage (e.g., erosive esophagitis, Barrett’s esophagus).
- Regular Check-ups: Monitoring symptoms, medication effectiveness, and any changes in esophageal health are important for long-term management.
5. Management of Complications:
- Barrett’s Esophagus: Monitoring with regular endoscopies and possibly treating with medication or ablation therapy to reduce the risk of esophageal cancer.
- Esophageal Strictures: Dilation procedures may be necessary to widen narrowed areas of the esophagus caused by chronic inflammation and scarring.
6. Patient Education and Support:
- Education: Providing information on GERD triggers, symptoms, and the importance of adherence to treatment.
- Support Groups: Offering support and resources for individuals coping with chronic GERD symptoms and management.