Hypoparathyroidism
content of this page
1- Introduction
2- Pathophysiological Overview
3- Symptoms
4- Treatment
Introduction
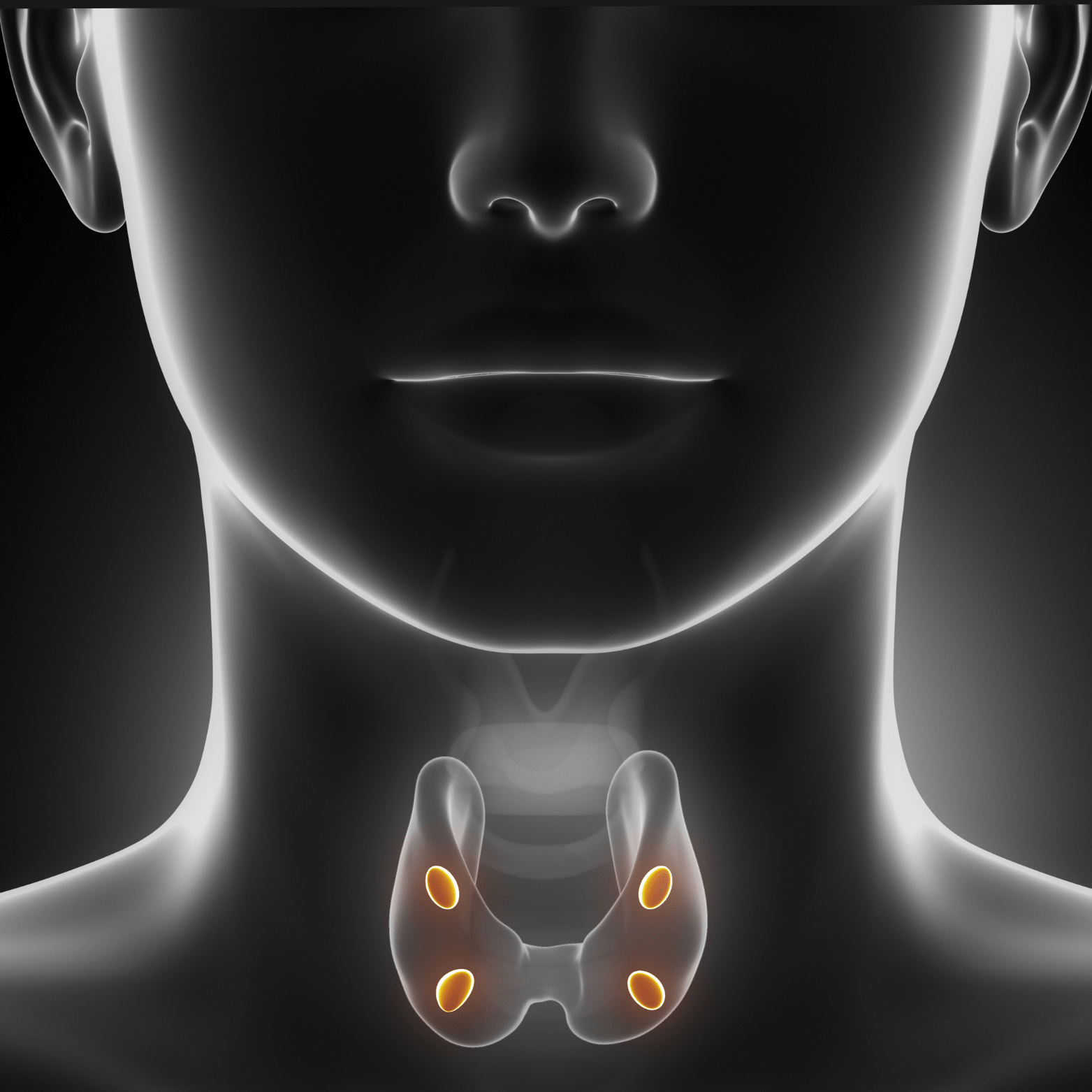
Hypoparathyroidism, characterized by abnormally low levels of parathyroid hormone (PTH), is primarily caused by damage to the parathyroid glands during thyroid surgery. Postoperative hypoparathyroidism affects approximately 0.5% to 6.6% of individuals undergoing thyroid surgery due to the close anatomical proximity of the parathyroid glands to the thyroid gland.
Other causes of hypoparathyroidism include:
Genetic Syndromes: Such as familial hypoparathyroidism and DiGeorge syndrome (velocardiofacial syndrome), where the parathyroid glands are underdeveloped or absent from birth.
Hypomagnesemia: Low levels of magnesium can impair PTH secretion and function, contributing to hypoparathyroidism.
Idiopathic or Autoimmune Forms: In some cases, the cause of hypoparathyroidism may be unknown or related to autoimmune disorders where the immune system attacks the parathyroid glands.
Pathophysiological Overview
In hypoparathyroidism a lack of circulating PTH causes a depressed serum calcium level
and an increased serum phosphate level. In the absence of PTH the abilities to resorb calcium from bone and to regulate calcium reabsorption from the renal tubules are impaired. The phosphaturic effects of PTH are lost, resulting in hyperphosphatemia. The effects of hypomagnesemia on the peripheral metabolism
and clearance of PTH are not clearly understood. Once serum magnesium levels return to normal, however, PTH secretion returns to normal, as does peripheral tissues’ responsiveness
to PTH. Hypomagnesemia may be related to chronic alcoholism, malnutrition, malabsorption, increased renal clearance of magnesium caused by the use of aminoglycoside antibiotics or certain chemotherapeutic agents, or prolonged magnesium-deficient parenteral nutritional therapy.
Symptoms
Neuromuscular Symptoms:
- Tingling and Numbness: Especially around the lips, fingers, and toes (paresthesias).
- Muscle Cramps and Spasms: Painful contractions, often in the hands, feet, or face.
- Tetany: Involuntary muscle contractions, causing spasms or cramps throughout the body.
- Chvostek’s Sign: Facial muscle twitching when the facial nerve is tapped.
- Trousseau’s Sign: Carpal spasm when a blood pressure cuff is inflated above systolic pressure for a few minutes.
Central Nervous System Symptoms:
- Headaches: Often severe and persistent.
- Seizures: Particularly in severe cases due to low calcium affecting nerve function.
- Mental Confusion: Cognitive difficulties, memory impairment, and mood changes.
Cardiovascular Symptoms:
- Arrhythmias: Irregular heart rhythms, palpitations, or fainting spells.
Other Symptoms:
- Dry Hair and Skin: Decreased moisture and increased susceptibility to dermatological issues.
- Brittle Nails: Nails that are fragile and prone to breakage.
- Dental Problems: Increased risk of dental enamel defects and cavities.
Treatment
1. Calcium Supplementation:
- Calcium Carbonate or Calcium Citrate: Oral calcium supplements are typically prescribed to increase calcium levels in the blood. The dosage is adjusted based on the severity of hypocalcemia and individual patient response.
2. Active Vitamin D (Calcitriol) or Analogues:
- Calcitriol (1,25-dihydroxyvitamin D): This active form of vitamin D helps the intestines absorb calcium from food and supplements. Analogues like alfacalcidol (1-alpha-hydroxyvitamin D3) may also be used.
3. Magnesium Supplementation:
- Magnesium Replacement: If hypomagnesemia (low magnesium levels) is contributing to hypoparathyroidism, magnesium supplements may be necessary to optimize PTH function and calcium metabolism.
4. Monitoring and Adjustments:
- Regular Blood Tests: Monitoring of calcium, phosphate, and PTH levels to assess treatment effectiveness and adjust medication dosages as needed.
5. Symptomatic Treatment:
Calcium Infusions: In severe cases or during acute episodes of tetany or seizures, intravenous calcium may be administered under medical supervision.
Management of Symptoms: Addressing neuromuscular symptoms such as muscle cramps or spasms with calcium supplements and sometimes additional medications like magnesium or anticonvulsants.
6. Lifestyle and Dietary Adjustments:
Dietary Calcium and Vitamin D: Encouraging calcium-rich foods and ensuring adequate vitamin D intake through diet or supplements.
Hydration: Maintaining good hydration status to prevent kidney stone formation, which can be a complication of long-term calcium supplementation.
7. Long-Term Care:
Regular Follow-up: Periodic visits to healthcare providers to monitor calcium levels, adjust medications, and assess for complications such as kidney stones or osteoporosis.
Patient Education: Educating patients about the signs and symptoms of hypocalcemia, the importance of medication adherence, and when to seek medical attention for complications.