Multinodular Goiter
Content of This Page
1- Introduction
2- Causes
3- Symptoms
4- Investigations & Lab Results
5- Prognosis
6- Treatment
Introduction
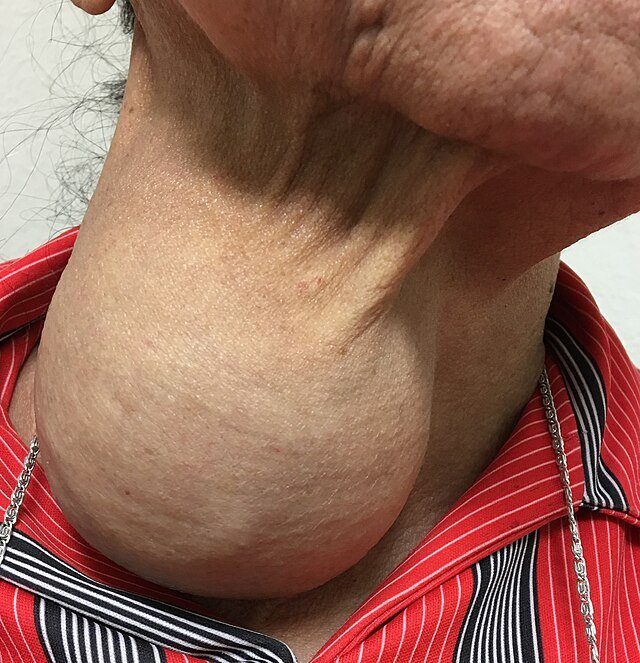
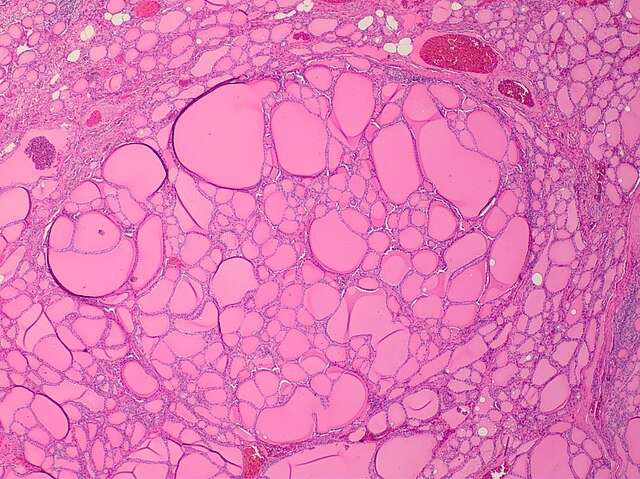
Multinodular Goiter is an enlargement of the thyroid gland characterized by the presence of multiple nodules within the gland. It is a common thyroid disorder that develops over time, often due to prolonged iodine deficiency, genetic factors, or other thyroid-stimulating influences. Unlike a simple diffuse goiter, a multinodular goiter has an irregular, lumpy texture because of the multiple nodules that may vary in size and consistency.
These nodules can be benign or, less commonly, malignant. Multinodular goiters may cause visible swelling in the neck and sometimes lead to symptoms from compression of nearby structures, such as difficulty swallowing or breathing.
Causes
Iodine deficiency: The most common cause worldwide; low iodine intake leads to thyroid stimulation and nodule formation.
Genetic predisposition: Family history of goiter or nodular thyroid disease.
Repeated episodes of thyroid hyperplasia and involution: Due to chronic stimulation by thyroid-stimulating hormone (TSH).
Thyroiditis: Chronic inflammation of the thyroid may contribute to nodule development.
Environmental factors: Exposure to goitrogens (certain foods, chemicals) that interfere with thyroid hormone synthesis.
Autonomous thyroid nodules: Some nodules gain the ability to function independently of TSH regulation, promoting growth.
Aging: Increased risk of multinodular goiter with advancing age.
Radiation exposure: Previous neck irradiation may increase risk.
Symptoms
Symptoms of Multinodular Goiter
Visible neck swelling: Gradual, painless enlargement of the thyroid gland with an irregular, lumpy texture
Compression symptoms (if large):
Difficulty swallowing (dysphagia)
Breathing difficulties or shortness of breath (dyspnea)
Hoarseness or voice changes (due to recurrent laryngeal nerve compression)
Sensation of tightness or fullness in the neck
Thyroid function-related symptoms:
Usually euthyroid (normal thyroid function)
Sometimes hyperthyroidism symptoms if toxic nodules develop, such as:
Weight loss
Heat intolerance
Palpitations
Nervousness or irritability
Tremors
No symptoms: Many multinodular goiters are asymptomatic and discovered incidentally during routine exams or imaging
Investigations & Lab Results
Thyroid Function Tests:
TSH:
Normal (euthyroid) in most cases
Suppressed if toxic nodules cause hyperthyroidism
Free T4 and Free T3:
Normal in euthyroid patients
Elevated in toxic multinodular goiter (hyperthyroid state)
Thyroid Antibodies:
Usually negative (helps differentiate from autoimmune thyroid diseases like Hashimoto’s or Graves’)
Thyroid Ultrasound:
Multiple nodules of varying size and echogenicity
May show cystic or solid components
Fine Needle Aspiration Cytology (FNAC):
Performed if suspicious nodules are present to rule out malignancy
Radioactive Iodine Uptake Scan:
Shows patchy uptake with “hot” (functioning) and “cold” (non-functioning) nodules in toxic multinodular goiter
Prognosis
Generally good, especially if diagnosed early and monitored regularly.
Many patients remain euthyroid with stable goiter size for years without complications.
Some goiters may grow slowly over time, potentially causing compressive symptoms requiring treatment.
Risk of developing hyperthyroidism (toxic multinodular goiter) increases with time, especially in iodine-deficient areas.
Rarely, nodules may harbor or develop thyroid cancer, so ongoing surveillance is important.
With appropriate treatment (medical, radioactive iodine, or surgery), most patients have favorable outcomes and good quality of life.
Untreated large goiters causing airway or swallowing problems can lead to serious complications.
Treatment
1. Observation and Monitoring
For small, asymptomatic, euthyroid multinodular goiters.
Regular follow-up with physical exams, thyroid function tests, and ultrasound.
2. Medical Treatment
Thyroid hormone suppression therapy:
Use of levothyroxine to suppress TSH and potentially reduce goiter size (controversial and less commonly used).
Iodine supplementation:
Effective in iodine-deficient areas to prevent further enlargement.
3. Radioactive Iodine Therapy
Used to shrink goiters, especially toxic multinodular goiter causing hyperthyroidism.
Helps reduce thyroid volume and control hyperthyroidism.
4. Surgery (Thyroidectomy)
Indications include:
Large goiters causing compressive symptoms (difficulty swallowing, breathing)
Suspicion or confirmation of malignancy
Cosmetic concerns
Toxic multinodular goiter not controlled by medical or radioactive iodine therapy
5. Treatment of Hyperthyroidism
If toxic nodules cause hyperthyroidism, treatment options include antithyroid drugs, radioactive iodine, or surgery.