Papillary Carcinoma
Content of This Page
1- Introduction
2- Causes
3- Symptoms
4- Investigations & Lab Results
5- Prognosis
6- Treatment
Introduction
Papillary Carcinoma of the Thyroid is the most common type of thyroid cancer, accounting for about 80% of all thyroid malignancies. It arises from the follicular cells of the thyroid gland and is characterized by slow growth and an excellent prognosis when detected early. This carcinoma typically presents as a painless thyroid nodule and often affects younger adults, especially women. It tends to spread to regional lymph nodes in the neck but rarely metastasizes to distant organs.

Causes
Radiation exposure:
Childhood or neck irradiation is the strongest known risk factor.
Genetic mutations:
Common mutations include RET/PTC rearrangements and BRAF mutations that drive tumor development.
Family history:
A family history of thyroid cancer increases risk.
Iodine intake:
Both iodine deficiency and excess have been implicated in thyroid cancer risk in some populations.
Chronic thyroiditis:
Conditions like Hashimoto’s thyroiditis may slightly increase the risk.
Environmental factors:
Exposure to certain chemicals or carcinogens may contribute, though evidence is limited.
Symptoms
Painless, gradually enlarging thyroid nodule or lump in the neck
Palpable firm mass in the thyroid region
Enlarged lymph nodes in the neck (cervical lymphadenopathy)
Hoarseness or voice changes (if the tumor affects the recurrent laryngeal nerve)
Difficulty swallowing or breathing (usually in advanced cases due to compression)
Generally, no symptoms of thyroid hormone imbalance (patients are usually euthyroid)
Investigations & Lab Results
Thyroid Function Tests:
Typically normal (patients are usually euthyroid)
TSH, Free T4, and Free T3 levels within normal limits
Neck Ultrasound:
Solid, hypoechoic thyroid nodule with irregular or ill-defined margins
Presence of microcalcifications (tiny bright spots)
Increased blood flow on Doppler imaging
Possible cervical lymph node enlargement
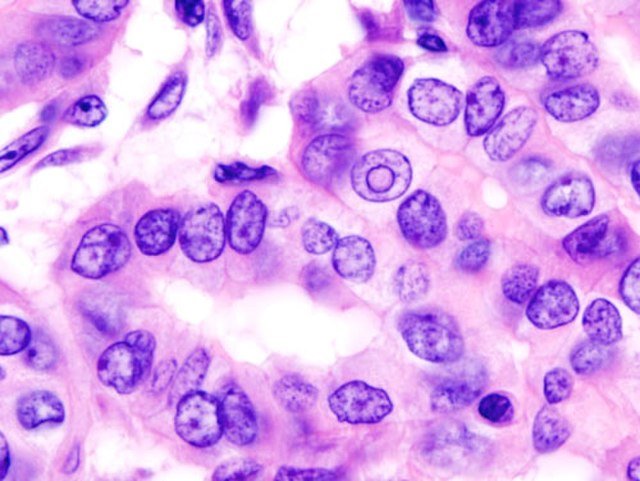
Fine Needle Aspiration Cytology (FNAC):
Key diagnostic tool
Shows characteristic features such as:
Orphan Annie eye nuclei (clear nuclei)
Nuclear grooves
Psammoma bodies (calcified structures)
Helps distinguish papillary carcinoma from benign nodules
Radioactive Iodine Scan:
Shows “cold” nodule corresponding to the tumor (area of decreased iodine uptake)
Primarily used after surgery to detect residual or metastatic disease
Cross-sectional Imaging (CT/MRI):
Used if local invasion or distant metastases are suspected
Serum Thyroglobulin:
Used as a tumor marker to monitor disease recurrence after thyroidectomy
Prognosis
Generally excellent, with a high survival rate—over 90% 10-year survival in most cases.
Slow-growing tumor with a tendency for local spread rather than distant metastasis.
Prognosis is better in younger patients (under 45 years) and those with small, localized tumors.
Cervical lymph node involvement is common but does not significantly worsen the prognosis.
Distant metastases (e.g., to lungs or bones) are rare but can affect outcomes.
Recurrence can occur but is often manageable with further treatment.
Early diagnosis and appropriate treatment (surgery with or without radioactive iodine) lead to very favorable outcomes.
Treatment
Surgery:
Total or near-total thyroidectomy is the mainstay of treatment.
Removal of involved cervical lymph nodes (lymph node dissection) if metastasis is present.
Radioactive Iodine (RAI) Therapy:
Used after surgery to ablate residual thyroid tissue and treat microscopic disease.
Helps reduce recurrence risk and facilitate follow-up using thyroglobulin as a tumor marker.
Thyroid Hormone Replacement Therapy:
Lifelong levothyroxine to maintain normal metabolism and suppress TSH, which can stimulate tumor growth.
External Beam Radiation Therapy:
Reserved for inoperable cases or when there is extensive local invasion not amenable to surgery.
Targeted Therapy or Chemotherapy:
Rarely needed; used in advanced, refractory cases.
Regular Follow-up:
Includes physical exams, ultrasound, serum thyroglobulin levels, and periodic imaging to detect recurrence.