Paroxysmal Nocturnal Hemoglobinuria (PNH)
Content of This Page
1- Introduction, Definition
2- Pathophysiology
3-Clinical Features
4- Investigations
5-Management
6- Prognosis
Introduction
PNH is a rare acquired clonal disorder of haematopoietic stem cells characterized by:
Deficiency of GPI (glycosylphosphatidylinositol)-anchored proteins on cell surfaces
Leading to complement-mediated intravascular haemolysis
It is non-malignant, but life-threatening due to risks of thrombosis and bone marrow failure.
Pathophysiology
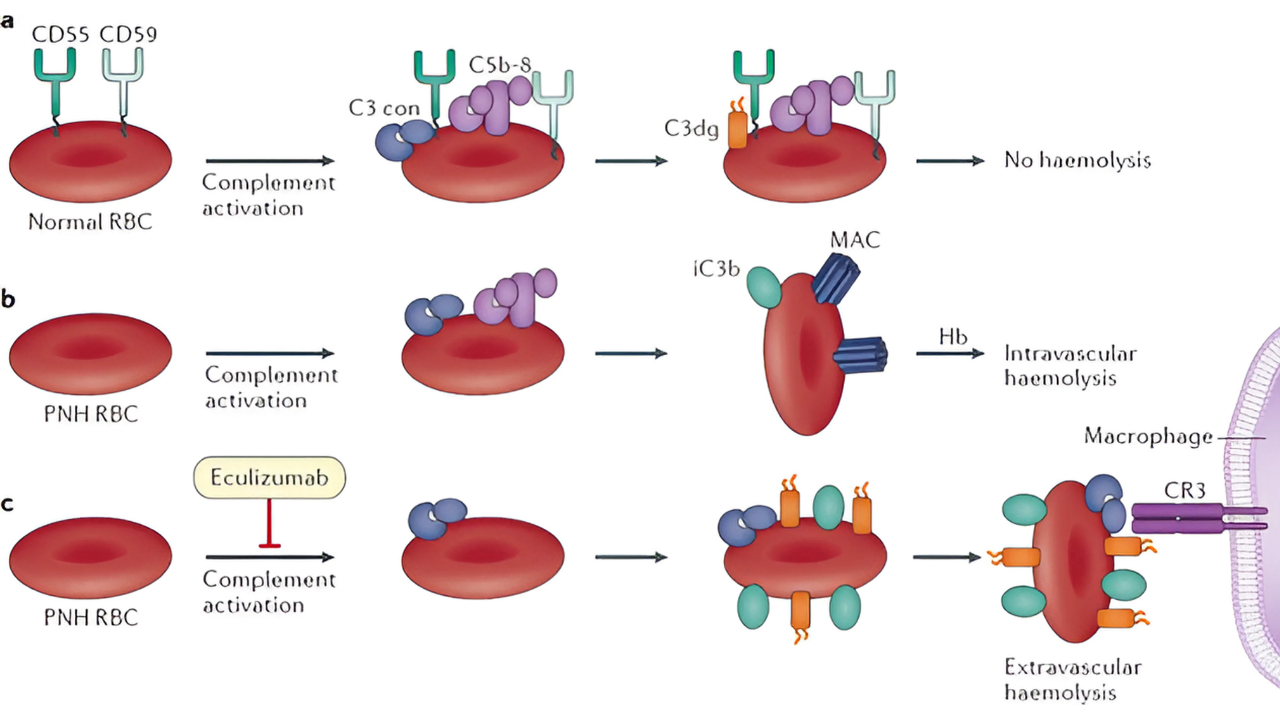
Mutation in PIGA gene → defective GPI anchors
GPI is needed to attach protective proteins (like CD55 and CD59) to red cell membranes
Loss of these proteins → red cells become hypersensitive to complement lysis
Leads to intravascular haemolysis, especially at night (when pH drops) → haemoglobinuria

Clinical Features
Classic triad:
Intravascular haemolysis → dark urine, especially in the morning (haemoglobinuria)
Thrombosis (major cause of mortality)
In unusual sites: hepatic veins (Budd–Chiari), cerebral, mesenteric
Bone marrow failure
Aplastic anaemia, pancytopenia, or overlap with myelodysplastic syndromes (MDS)
-Others:
Fatigue, dyspnoea (from anaemia)
Jaundice, abdominal pain (from haemolysis)
Investigations
Haemolysis markers:
↓ Haemoglobin
↑ LDH, indirect bilirubin, reticulocytes
↓ Haptoglobin
Haemoglobinuria ± positive urinary haemosiderin
Confirmatory test:
Flow cytometry: absence of CD55/CD59 on red/white cells
(GPI-anchored surface proteins)
Management
Supportive care:
Blood transfusions (cautious crossmatching)
Folic acid supplementation
Thrombosis prophylaxis/treatment (low threshold for anticoagulation)
–Disease-modifying therapy:
Eculizumab or ravulizumab (anti-C5 monoclonal antibodies)
Reduce haemolysis, transfusion needs, and thrombosis risk
Increase risk of meningococcal infection → vaccination required
–Bone marrow transplant:
Considered in severe bone marrow failure or resistant disease
Prognosis
Variable, depending on:
Degree of haemolysis
Risk and management of thrombosis
Presence of bone marrow failure
With C5 inhibitors, outcomes are significantly improved