Systemic Lupus Erythematosus (SLE)
Content of This Page
1- Introduction
2- Causes
3- Symptoms
4- Stages of The Disease
5- Treatment
6- What Should You Avoid
Introduction
Systemic Lupus Erythematosus (SLE) is a long-term autoimmune disease in which the body’s immune system mistakenly attacks its own tissues. This leads to inflammation and damage in various organs, including the skin, joints, kidneys, and heart. Symptoms often include joint pain, skin rashes, fatigue, and fever. SLE is a chronic condition that requires treatment to manage symptoms and reduce flare-ups.
Causes
Genetics: If allergies run in your family, you’re more likely to develop them yourself.
Environmental Exposure: Exposure to allergens like pollen, dust mites, mold, pet dander, or certain foods can trigger allergic reactions.
Immune System Response: In individuals with allergies, the immune system mistakenly identifies harmless substances as threats and produces an exaggerated response.
Hygiene Hypothesis: Some research suggests that less exposure to infections in early childhood may increase the likelihood of developing allergies. This theory proposes that a lack of exposure to certain germs and microbes can lead to an overactive immune system.
Environmental Changes: Increased pollution and changes in climate can also contribute to the rise in allergies.
Symptoms
- Fatigue
- Joint Pain and Swelling
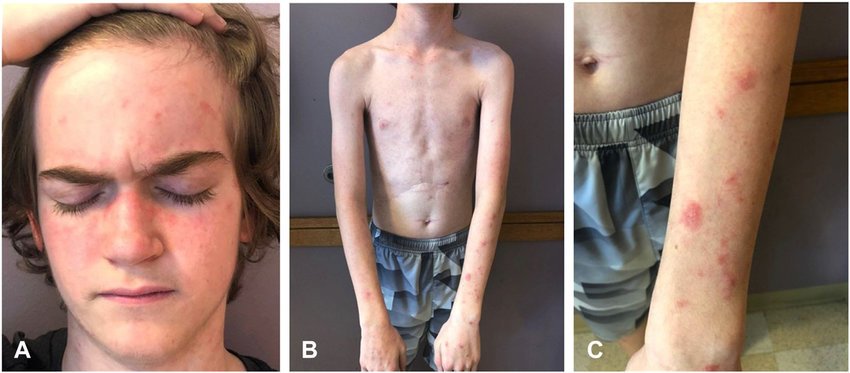
- Skin Rash: Often a butterfly-shaped rash across the cheeks and nose.
- Fever
- Hair Loss
- Photosensitivity: Sensitivity to sunlight leading to rashes or flare-ups.
- Mouth or Nasal Ulcers
- Chest Pain: Due to inflammation of the lining of the heart or lungs.
- Kidney Problems: Symptoms may include swelling of the legs or high blood pressure.
- Raynaud’s Phenomenon: Fingers and toes turning white or blue in response to cold or stress.

Stages of The Disease
Initial Onset:
- Early symptoms may include fatigue, joint pain, and mild rashes. This stage often involves the first appearance of symptoms, which can be vague and nonspecific.
Active Phase:
- Symptoms become more pronounced and involve multiple organ systems. This phase may include severe flare-ups with increased inflammation, affecting skin, joints, kidneys, and other organs.
Remission:
- Periods where symptoms decrease or disappear, often due to effective treatment or spontaneous remission. Patients may experience reduced disease activity and improved quality of life.
Chronic Phase:
- Long-term management is necessary. Symptoms may persist at a lower intensity, and ongoing treatment aims to manage and prevent flare-ups and complications.
Flare-ups:
- Intermittent periods of increased disease activity where symptoms worsen. Management focuses on controlling symptoms and preventing organ damage.
Treatment
Medications:
- Nonsteroidal Anti-Inflammatory Drugs (NSAIDs): For pain and inflammation.
- Antimalarials: Such as hydroxychloroquine to control skin rashes and joint pain.
- Corticosteroids: To reduce inflammation during flare-ups.
- Immunosuppressants: Drugs like azathioprine or mycophenolate to suppress the immune system and reduce disease activity.
- Biologics: Target specific parts of the immune system, used for more severe cases.
Lifestyle Modifications:
- Sun Protection: Avoiding direct sunlight and using sunscreen to prevent skin flare-ups.
- Healthy Diet: Eating a balanced diet to support overall health.
- Regular Exercise: To maintain joint and cardiovascular health.
Monitoring and Regular Check-Ups:
- Regular visits to a healthcare provider to monitor disease activity and manage complications.
Managing Specific Symptoms:
- Kidney Issues: Treatment may include medications specific to kidney function.
- Heart or Lung Involvement: Specialized treatment for any cardiovascular or respiratory symptoms.
Supportive Care:
- Mental Health Support: Counseling or therapy to manage the emotional impact of chronic
What Should You Avoid
- Excessive Sun Exposure: Use sunscreen and wear protective clothing.
- Smoking: Can worsen symptoms and increase complications.
- Infections: Practice good hygiene and avoid exposure to illness, as infections can trigger flare-ups.
- Stress: Manage stress through relaxation techniques and support.
- Certain Medications: Avoid medications that can exacerbate symptoms, such as those that are not recommended by your healthcare provider.
- Excessive Physical Activity: Balance exercise with rest to avoid overexertion.
- Known Allergens or Triggers: Identify and avoid substances that trigger your symptoms.