Myasthenia Gravis
content of this page
1- Introduction
2- Pathophysiology
3- Symptoms
4- Treatment
Introduction
Myasthenia gravis is a chronic autoimmune disease mediated by acetylcholine receptor (AChR) antibodies that act at the neuromuscular junction; it affects 20,000 to 70,000 people in the United States. The disease is characterized by exertional fatigue and weakness that worsens with activity, improves with rest, and recurs with resumption of activity.

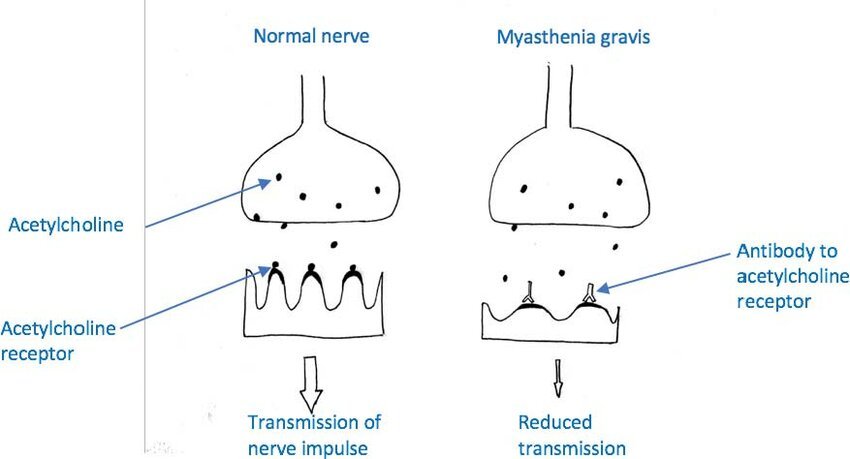
Pathophysiology
Myasthenia gravis results from a defect in nerve impulse transmission at the neuromuscular junction. The main defect is the formation of autoantibodies (an IgG antibody) against receptors at the ACh binding site on the postsynaptic membrane. The autoantibodies block the AChR or cause complement-mediated loss of AChRs from the neuromuscular junction. The cause of this autosensitization is not known. Eventually the destruction of receptor sites occurs, and the number of receptors on the plasma membrane is reduced. The destruction of receptor sites causes diminished transmission of nerve impulses across the neuromuscular junction. Muscle depolarization is incomplete or not achieved.
Symptoms
Myasthenia gravis (MG) is a chronic autoimmune disorder that affects the neuromuscular junction, causing muscle weakness and fatigue. The symptoms of myasthenia gravis can vary widely among individuals and may include:
Muscle Weakness: One of the hallmark symptoms of myasthenia gravis is muscle weakness that worsens with activity and improves with rest. This weakness can affect various muscles but commonly involves the muscles that control eye movements, facial expressions, chewing, swallowing, and speaking.
Ptosis: Drooping of one or both eyelids (ptosis) is a common early symptom in many people with myasthenia gravis. Ptosis can vary in severity and may worsen throughout the day as muscles become fatigued.
Diplopia: Double vision (diplopia) often occurs due to weakness or paralysis of the muscles that control eye movement. This symptom may worsen with prolonged use of the eyes (e.g., reading or driving).
Facial Weakness: Weakness in the facial muscles can lead to difficulty smiling, chewing, and maintaining facial expressions. This can contribute to a “masked” or expressionless facial appearance.
Difficulty Swallowing (Dysphagia): Weakness in the muscles involved in swallowing (pharyngeal and esophageal muscles) can cause difficulty swallowing liquids and solids, which may lead to choking or aspiration.
Weakness in Limbs: Some individuals with myasthenia gravis may experience weakness in the arms, hands, legs, or neck muscles, which can affect mobility and daily activities.
Breathing Difficulties: In severe cases, weakness of the respiratory muscles (diaphragm and intercostal muscles) can lead to breathing difficulties, especially during physical exertion or at night. This is considered a medical emergency and requires immediate attention.
Fatigue: Generalized fatigue is common in myasthenia gravis, often exacerbated by muscle weakness and the effort required to compensate for weakened muscles.
Speech Changes: Weakness in the muscles involved in speech production (such as the tongue and lips) can lead to slurred speech or difficulty articulating words clearly.
Change in Facial Expression: Difficulty maintaining a steady gaze or smiling due to muscle weakness in the facial muscles.
Exacerbation of Symptoms: Symptoms of myasthenia gravis can worsen with physical exertion, illness, stress, or certain medications that affect neuromuscular function.
Treatment
The treatment of myasthenia gravis (MG) aims to improve muscle strength, manage symptoms, and achieve remission of the autoimmune response. Treatment approaches may vary depending on the severity of symptoms, the specific manifestations of MG in each individual, and other factors such as age and overall health. Here are the primary treatment options for myasthenia gravis:
Medications:
- Cholinesterase Inhibitors: Medications such as pyridostigmine (Mestinon) are commonly used to improve neuromuscular transmission by preventing the breakdown of acetylcholine, a neurotransmitter that signals muscle contraction.
- Immunosuppressants: Drugs like corticosteroids (e.g., prednisone) and other immunosuppressive agents (e.g., azathioprine, mycophenolate) may be prescribed to suppress the autoimmune response that attacks the neuromuscular junction.
- Monoclonal Antibodies: Biologic therapies such as rituximab or eculizumab target specific components of the immune system to reduce antibody production or inhibit complement-mediated damage.
Thymectomy:
- Surgical removal of the thymus gland (thymectomy) is recommended for some individuals, particularly those with thymoma (a tumor of the thymus) or younger patients with generalized MG. Thymectomy can lead to improved symptoms and potentially induce remission in some cases.
Plasma Exchange (Plasmapheresis) and Intravenous Immunoglobulin (IVIg):
- These treatments are used in severe cases or during myasthenic crises to rapidly reduce circulating antibodies or replace pathogenic antibodies with normal immunoglobulins, temporarily improving muscle strength.
Symptomatic Treatments:
- Eyelid Surgery: Surgical correction of ptosis (drooping eyelids) and strabismus (eye misalignment) may be considered to improve vision and quality of life.
- Speech and Swallowing Therapy: Techniques and exercises to improve speech clarity and swallowing function may be beneficial, particularly for individuals with bulbar symptoms.
Respiratory Support:
- Some individuals with myasthenia gravis, particularly those with respiratory muscle weakness, may require intermittent or continuous respiratory support, such as non-invasive ventilation (e.g., bilevel positive airway pressure, BiPAP) or mechanical ventilation in severe cases.
Management of Triggers:
- Avoiding factors that exacerbate MG symptoms, such as stress, fatigue, certain medications (e.g., antibiotics, muscle relaxants), and infections, can help manage the condition more effectively.
Regular Monitoring and Adjustments:
- Close monitoring of symptoms, medication effectiveness, and potential side effects is essential. Treatment plans may need adjustments over time to maintain optimal control of symptoms and minimize complications.
Multidisciplinary Care:
- Management of myasthenia gravis often involves a multidisciplinary team approach, including neurologists, immunologists, thoracic surgeons (for thymectomy), respiratory therapists, speech-language pathologists, and physical therapists.