Osteomyelitis
Content of This Page
1- Introduction
2- Causes
3- Symptoms
4- Types of Disease
5- Treatment
6- What Should You Avoid
Introduction
Osteomyelitis is an infection of the bone that can be caused by bacteria, fungi, or other microorganisms. It can affect any bone in the body but commonly involves the long bones of the arms and legs, the spine, or the pelvis. Osteomyelitis can be acute or chronic and may develop due to various factors or pre-existing conditions.

Causes
Bacterial Infection
- Most Common: Staphylococcus aureus, including methicillin-resistant Staphylococcus aureus (MRSA).
- Other Bacteria: Escherichia coli, Pseudomonas aeruginosa, and Streptococcus species.
- Source: Bacteria can enter the bone through an open wound, surgery, or from an infection elsewhere in the body.
Fungal Infection
- Types: Can be caused by fungi such as Candida species or Aspergillus species.
- Risk Factors: More common in individuals with weakened immune systems or those who have undergone recent surgery.
Mycobacterial Infection
- Types: Caused by Mycobacterium tuberculosis (tuberculous osteomyelitis) or other mycobacterial species.
- Source: Often associated with tuberculosis or disseminated infections.
Hematogenous Spread
- Description: Infection spreads to the bone from another part of the body through the bloodstream.
- Source: Can occur with conditions such as bacterial endocarditis or septicemia.
Direct Contamination
- Description: Infection enters the bone through an open fracture, surgical wound, or as a result of trauma.
- Source: Often related to external injuries or surgical procedures.
Chronic Conditions
- Description: Conditions like diabetes, vascular disease, or chronic kidney disease can increase the risk of osteomyelitis.
- Impact: Weakened immune response or compromised blood flow may contribute to infection.
Symptoms
Acute Osteomyelitis:
- Pain: Localized pain in the affected bone.
- Swelling and Redness: Swelling, redness, and warmth at the infection site.
- Fever: High fever and chills.
- General Malaise: Fatigue and general feeling of illness.
Chronic Osteomyelitis:
- Persistent Pain: Chronic pain in the affected area.
- Swelling: Ongoing swelling and tenderness.
- Sinus Tracts: Development of draining sores or sinus tracts near the infection site.
- Fever: Low-grade fever or no fever.
Types of Disease
1. Acute Osteomyelitis
- Onset: Develops suddenly, usually within a few days to weeks.
- Characteristics: Often caused by a bacterial infection, leading to rapid onset of symptoms like severe pain, swelling, and fever.
- Common Causes:
- Hematogenous Spread: Infection spread through the bloodstream.
- Direct Contamination: Infection entering through an open wound or surgical site.
2. Chronic Osteomyelitis
- Onset: Develops gradually, typically persisting for months or years.
- Characteristics: Often associated with a long-standing infection that has led to persistent symptoms and may involve the formation of bone abscesses or sinus tracts (draining sores).
- Common Causes:
- Chronic Conditions: Diabetes, vascular disease, or immunosuppression.
- Previous Acute Infection: Inadequately treated or recurrent acute osteomyelitis.
3. Hematogenous Osteomyelitis
- Location: Affects bones through the bloodstream.
- Characteristics: Often seen in children, where bacteria from infections elsewhere in the body travel through the bloodstream to infect the bone.
- Common Causes:
- Bacterial Infections: Such as Staphylococcus aureus or Streptococcus species.
- Associated Conditions: Endocarditis or septicemia.
4. Contiguous Focus Osteomyelitis
- Location: Results from infection spreading from adjacent tissues or structures.
- Characteristics: Typically develops as a complication of infections in nearby tissues or from external sources such as open fractures or surgical wounds.
- Common Causes:
- Trauma or Surgery: Open fractures, surgical wounds, or pressure sores.
- Adjacent Infections: Infections from soft tissues or skin.
5. Post-Traumatic Osteomyelitis
- Location: Develops after a bone injury or surgical procedure.
- Characteristics: Infection results from an external injury, such as a fracture or surgical wound.
- Common Causes:
- Open Fractures: Where the bone is exposed to the environment.
- Surgical Complications: Infections following orthopedic surgeries or procedures.
6. Post-Surgical Osteomyelitis
- Location: Occurs following surgical procedures involving bones or adjacent tissues.
- Characteristics: May be a complication of surgery, particularly in cases where infection control measures are inadequate.
- Common Causes:
- Surgical Wounds: Infections following bone surgery or joint replacement.
7. Tuberculous Osteomyelitis
- Location: Caused by Mycobacterium tuberculosis.
- Characteristics: Often associated with systemic tuberculosis infection and can affect any bone.
- Common Causes:
- Spread from Pulmonary Tuberculosis: Mycobacterial infection spreading from the lungs to the bones.
8. Fungal Osteomyelitis
- Location: Caused by fungi, less common than bacterial osteomyelitis.
- Characteristics: More likely to occur in immunocompromised individuals or those with systemic fungal infections.
- Common Causes:
- Fungal Infections: Candida species, Aspergillus species.
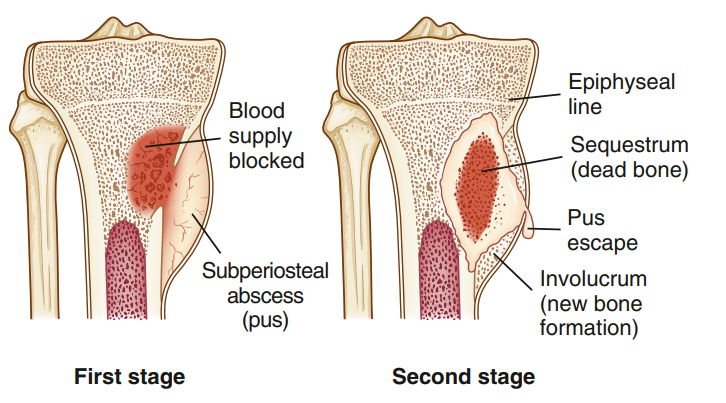
9. Chronic Suppurative Osteomyelitis
- Location: A form of chronic osteomyelitis characterized by the presence of pus and ongoing infection.
- Characteristics: Includes chronic inflammation and the formation of abscesses within the bone.
10. Osteomyelitis Associated with Systemic Conditions
- Location: Can be seen in patients with chronic systemic diseases.
- Characteristics: May occur as a complication of conditions such as diabetes mellitus, chronic kidney disease, or immunosuppression.
Treatment
Antibiotics
- Approach: Administered intravenously or orally, depending on the severity and type of infection.
- Duration: Typically requires several weeks of antibiotic therapy.
- Adjustments: Antibiotic choice may be adjusted based on culture results and response to treatment.
Surgery
- Approach: May be necessary to remove infected or dead tissue, drain abscesses, or correct structural abnormalities.
- Types: Surgical debridement to remove necrotic tissue and infected bone.
Pain Management
- Medications: Pain relief through medications such as NSAIDs or analgesics.
Supportive Care
- Wound Care: Proper care of wounds or surgical sites to prevent further infection.
- Rehabilitation: Physical therapy and rehabilitation to restore function and mobility.
Treatment of Underlying Conditions
- Management: Addressing underlying health issues such as diabetes or vascular disease to support overall recovery and prevent recurrence.
What Should You Avoid
- Wound Care: Proper cleaning and care of cuts, wounds, or surgical sites.
- Infection Control: Following good hygiene practices and using sterile techniques during medical procedures.
- Management of Chronic Conditions: Effective management of conditions that may increase the risk of infection.
- Prompt Medical Attention: Seeking medical advice for persistent symptoms or signs of infection.