Impetigo
Content of This Page
1- Introduction
2- Causes
3- Symptoms
4- Stages of The Disease
5- Treatment
6- What Should You Avoid
Introduction
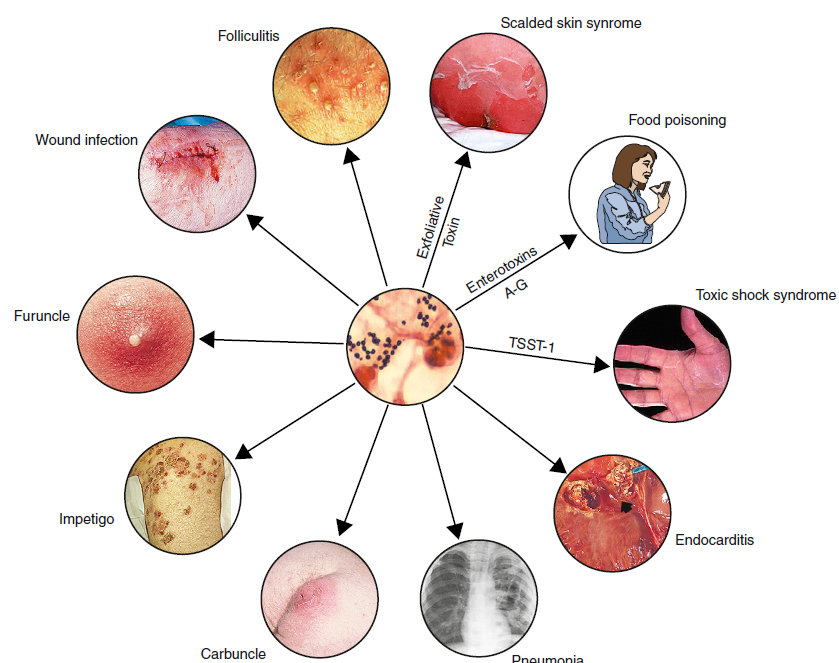
Impetigo is a highly contagious bacterial skin infection that primarily affects young children but can occur in individuals of any age. It causes red sores or blisters that can rupture, ooze, and form a yellowish-brown crust. The infection is usually caused by Staphylococcus aureus or Streptococcus bacteria

Causes
-Impetigo is caused by bacteria, most commonly:
- Staphylococcus aureus: A type of bacteria that frequently causes impetigo.
- Streptococcus pyogenes: Another common bacterial cause.
-The bacteria can enter the skin through:
- Cuts or Scrapes: Open wounds or minor injuries.
- Insect Bites: Bites that break the skin.
- Skin Conditions: Such as eczema or chickenpox, which can provide entry points for bacteria.
- Direct Contact: Touching infected skin or contaminated items.
Symptoms
- Red Sores or Blisters: Often appear around the nose, mouth, and on the face, but can occur elsewhere.
- Rupture and Oozing: Sores can burst, oozing a yellowish fluid.
- Crusting: The oozed fluid dries to form a thick, honey-colored crust.
- Itching: The affected area can be itchy.
- Swelling: Mild swelling around the infected area.
- Fever: In some cases, especially with more severe infections.
Stages of The Disease
Initial Infection:
- Symptoms: Red sores or blisters appear on the skin, often around the nose and mouth.
- Description: The bacteria begin to multiply, causing the initial appearance of sores.
Early Stage:
- Symptoms: Sores rupture and ooze a yellowish fluid.
- Description: The fluid from the sores starts to accumulate and the infection spreads to nearby skin.
Progressive Stage:
- Symptoms: The oozing fluid dries and forms a thick, honey-colored crust. The infection may spread to other parts of the body.
- Description: The crust forms as the fluid dries out, and the infection can continue to spread if not treated.
Resolution:
- Symptoms: Symptoms begin to improve with treatment, and the crusts gradually fall off. The skin heals, though it may remain red or discolored for some time.
- Description: The infection resolves with appropriate treatment, and the affected skin gradually returns to normal.
Treatment
Topical Antibiotics:
- Ointments or Creams: Such as mupirocin or retapamulin applied directly to the affected area.
Oral Antibiotics:
- Tablets or Capsules: For more widespread or severe cases, such as dicloxacillin or cephalexin.
Good Hygiene Practices:
- Cleaning the Area: Gently washing affected areas with soap and water.
- Keeping Sores Covered: Using clean, dry bandages to prevent spreading.
Avoiding Contact:
- Preventing Spread: Avoiding close contact with others and not sharing personal items.
Managing Itching:
- Over-the-Counter Antihistamines: To relieve itching if necessary.
Monitoring and Follow-Up:
- Regular Check-Ups: Ensuring the infection is responding to treatment and addressing any complications.
What Should You Avoid
- scratching or picking at sores.
- sharing personal items.
- close contact with others.
- using contaminated towels or bedding.
- stopping treatment early.