Scabies
Content of This Page
1- Introduction
2- Causes
3- Symptoms
4- Stages of Disease
5- Treatment
6- What Should You Avoid
Introduction
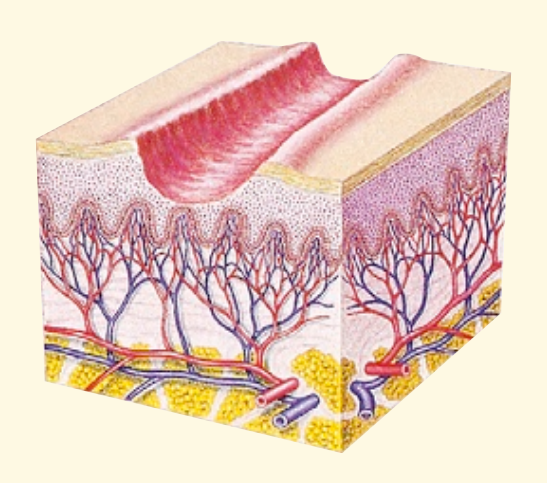
Scabies is a highly contagious skin condition caused by a tiny mite called Sarcoptes scabiei. These mites burrow into the skin, causing intense itching and a pimple-like rash. Scabies can affect people of all ages and socioeconomic backgrounds, and it is most commonly spread through close physical contact with an infected person.

Causes
Sarcoptes scabiei: The female mite burrows into the top layer of the skin to lay eggs, leading to the symptoms of scabies. The mites are not visible to the naked eye, but their presence causes a significant immune response, resulting in itching and rash.
Symptoms
- Intense Itching: The most common symptom, often worse at night.
- Rash: A pimple-like rash that may appear as tiny blisters or sores. The rash is typically found in skin folds, such as between the fingers, on the wrists, elbows, knees, around the waist, and on the buttocks.
- Burrows: Thin, grayish-white or skin-colored lines on the skin surface, which are the tracks created by the mites as they burrow.
- Sores: Scratching the itchy areas can cause sores, which may become infected.
- Crusting: In severe cases, particularly in immunocompromised individuals, scabies can cause thick crusts on the skin that contain large numbers of mites. This is known as crusted scabies (or Norwegian scabies) and is highly contagious.
Stages of Disease
1. Incubation Period
- Timeframe: 2 to 6 weeks after initial exposure (for a first-time infestation); symptoms can appear within a few days if you’ve had scabies before.
- Description: After the mites are transferred to the skin, they begin to burrow into the outer layer of the skin. During this period, the person may not notice any symptoms, as it takes time for the immune system to react to the mites. However, the person is still contagious and can spread the mites to others.
2. Early Stage (Initial Symptoms)
- Symptoms: Itching, especially at night, is usually the first noticeable symptom. This itching is a reaction to the mites, their eggs, and waste under the skin.
- Appearance: Small, pimple-like bumps or blisters may start to appear on the skin, often in areas where the mites have burrowed. Common areas include the webbing between the fingers, wrists, elbows, armpits, waist, buttocks, and around the nipples in women or genital area in men.
3. Progressive Stage
- Symptoms: The itching becomes more intense, especially at night, and the rash spreads to other parts of the body. The immune system’s response to the mites increases, leading to more noticeable skin changes.
- Appearance: The rash can develop into widespread, small, red bumps or vesicles (tiny blisters). Burrows may become visible as thin, irregular lines on the skin, often appearing grayish-white or skin-colored. Scratching the affected areas can cause sores or open wounds, which may lead to secondary bacterial infections.
4. Advanced Stage
- Symptoms: In untreated cases, the symptoms worsen over time. The itching can become unbearable, and the rash may spread further. Secondary bacterial infections from scratching can develop, leading to impetigo or other complications.
- Complications: Some people may develop more severe forms of scabies, such as crusted (Norwegian) scabies, where thick crusts form on the skin, containing thousands of mites. This form of scabies is particularly contagious and difficult to treat, often seen in immunocompromised individuals.
5. Post-Treatment Stage
- After Treatment: Once treatment begins, the mites are killed, but itching and skin irritation may persist for several weeks as the body continues to react to the dead mites and eggs.
- Symptoms: It’s common to experience “post-scabies itch” even after successful treatment. The rash and itching will gradually subside as the skin heals, and no new burrows should appear if the treatment was effective.
6. Resolution
- Symptoms: Over time, the skin will return to normal as it recovers from the infestation. Any secondary infections will also heal with appropriate treatment.
- Precaution: It’s important to follow up with a healthcare provider to ensure the infestation has been completely eradicated and to treat any lingering skin issues.
Treatment
- Topical Medications:
- Permethrin Cream: The most commonly prescribed treatment, applied to the entire body from the neck down and left on for 8-14 hours before washing off.
- Lindane Lotion: Used in cases where other treatments are ineffective, but it should be avoided in certain populations, such as pregnant women, infants, and the elderly.
- Crotamiton Cream or Lotion: Another option for those who cannot use permethrin.
- Oral Medications:
- Ivermectin: An oral medication used for severe cases or when topical treatments fail. It is particularly useful for treating crusted scabies.
- Treatment of Close Contacts: Because scabies is highly contagious, it is essential to treat all household members, sexual partners, and close contacts simultaneously, even if they are asymptomatic.
- Environmental Cleaning: Wash clothing, bedding, and towels in hot water and dry them on a hot cycle. Items that cannot be washed should be sealed in a plastic bag for at least 72 hours to kill the mites.
What Should You Avoid
1. Close Physical Contact
- Impact: Scabies is highly contagious and spreads easily through prolonged skin-to-skin contact.
- Avoid: Close physical contact with others, including hugging, holding hands, and sexual contact, until you have completed treatment and are cleared by a healthcare provider.
2. Sharing Personal Items
- Impact: Scabies mites can live on clothing, bedding, and towels, potentially spreading the infestation.
- Avoid: Sharing clothing, towels, bedding, or any personal items that come into direct contact with your skin.
3. Delaying Treatment
- Impact: The longer scabies goes untreated, the more it can spread to others and cause severe symptoms.
- Avoid: Ignoring symptoms or delaying treatment. Seek medical advice as soon as you suspect scabies.
4. Incomplete Treatment
- Impact: Not following through with the full course of treatment can lead to reinfestation and continued symptoms.
- Avoid: Stopping treatment early, even if symptoms seem to improve. Follow your healthcare provider’s instructions completely.
5. Contact with Infested Items
- Impact: Scabies mites can survive on items like bedding, clothing, and furniture for a short time, leading to reinfestation or spreading the mites to others.
- Avoid: Reusing unwashed bedding, clothing, and towels before they have been properly cleaned. Wash these items in hot water and dry them on a high heat setting.
6. Over-the-Counter Treatments Without Prescription
- Impact: Over-the-counter treatments may not be effective against scabies, and improper use can worsen the condition.
- Avoid: Using over-the-counter creams or lotions without consulting a healthcare provider. Prescription medications like permethrin cream or oral ivermectin are typically needed to effectively treat scabies.
7. Scratching
- Impact: Scratching the itchy areas can cause skin damage, leading to secondary bacterial infections.
- Avoid: Scratching as much as possible. Instead, use prescribed anti-itch medications or home remedies like cool compresses to relieve itching.
8. Contact with Untreated Individuals
- Impact: If you have scabies, you can easily spread it to others who haven’t been treated.
- Avoid: Close contact with others who haven’t been treated, and ensure that all household members and close contacts are treated simultaneously.
9. Delaying Environmental Cleaning
- Impact: Scabies mites can live for a short period off the body, so it’s important to clean the environment to prevent reinfestation.
- Avoid: Skipping or delaying the cleaning of your environment. Vacuum furniture, wash bedding and clothing, and consider isolating items that can’t be washed for at least 72 hours.
10. Public Spaces and Shared Facilities
- Impact: Using shared facilities like gyms, pools, or saunas can increase the risk of spreading scabies to others.
- Avoid: Public spaces and shared facilities until you have completed treatment and are no longer contagious.