Metastatic Lymph Node Involvement
Content of This Page
1- Introduction
2- Pathophysiology of Lymphatic Spread in Cancer
3- Common Primary Tumours Causing Nodal Metastases
4- Clinical Features of Metastatic Lymphadenopathy
5-Anatomical Patterns of Nodal Spread in Malignancy
6- Staging Systems Involving Lymph Nodes (e.g. TNM)
7- Radiological and Nuclear Imaging in Nodal Metastasis
8- Biopsy and Histopathological Confirmation
9- Management Principles in Nodal Metastatic Disease
10- Prognostic Implications of Nodal Involvement
Introduction
Lymph node metastasis occurs when malignant cells from a primary tumour spread via lymphatic vessels to regional or distant lymph nodes. This is a hallmark of solid organ malignancies, often serving as an early sign of cancer and a major component of cancer staging.
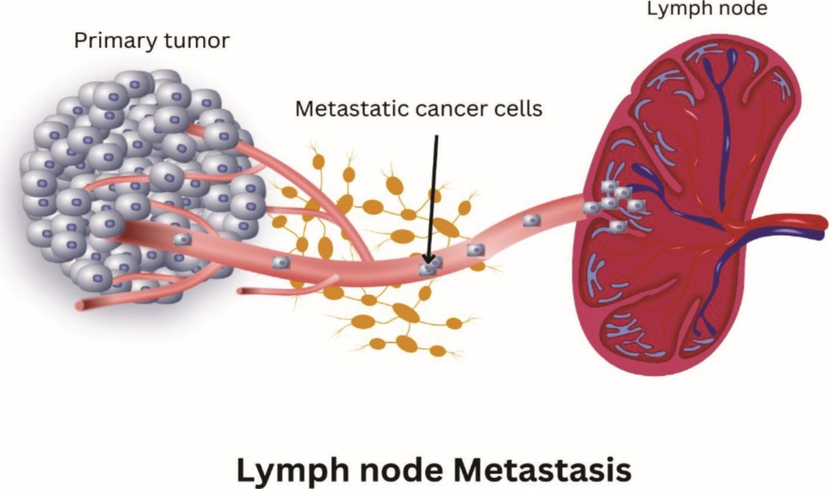
Pathophysiology of Lymphatic Spread in Cancer
Tumour cells invade afferent lymphatic channels near the primary site.
These cells are transported to regional lymph nodes, where they may:
Evade immune clearance
Proliferate and establish secondary deposits
Spread typically follows anatomical lymphatic drainage patterns
Lymphovascular invasion is a poor prognostic marker
Common Primary Tumours Causing Nodal Metastases
| Primary Site | Likely Nodes Involved |
|---|---|
| Lung | Hilar, mediastinal, supraclavicular (N1–N3) |
| Breast | Axillary, internal mammary, supraclavicular |
| Stomach | Perigastric, celiac, Virchow’s node (left supraclavicular) |
| Colorectal | Mesorectal, inferior mesenteric, para-aortic |
| Prostate/Bladder | Pelvic, para-aortic |
| Thyroid | Cervical, upper mediastinal |
| Head & Neck | Cervical (level I–V), retropharyngeal |
Clinical Features of Metastatic Lymphadenopathy
Painless, hard, non-tender nodes
Fixed to surrounding tissues
Unilateral and often progressive
Supraclavicular nodes (especially left = Virchow’s node) → suggests intra-abdominal or thoracic malignancy
May be first sign of an occult cancer
Anatomical Patterns of Nodal Spread in Malignancy
Spread often respects lymphatic drainage territories, e.g.:
Right supraclavicular node: intrathoracic disease
Left supraclavicular node (Virchow’s): abdominal malignancies
Axillary nodes: breast, upper limb
Inguinal: genital, anal, lower limb malignancies
Staging Systems Involving Lymph Nodes (TNM)
TNM = Tumour (T), Nodes (N), Metastasis (M)
N stage is based on:
Number of involved nodes
Size of metastases
Laterality (ipsilateral vs contralateral)
E.g. N1–N3 in lung or breast cancer has defined clinical cut-offs
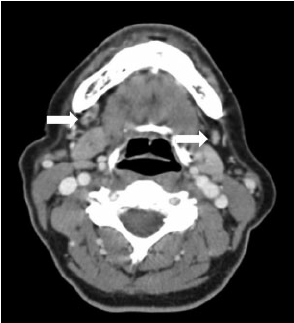
Radiological and Nuclear Imaging in Nodal Metastasis
CT scan: identifies enlarged or necrotic nodes
MRI: for soft tissue definition, especially head/neck and pelvic disease
PET-CT: detects metabolically active nodes → staging and monitoring
Ultrasound + FNAC: useful for superficial nodes (e.g. cervical)
Biopsy and Histopathological Confirmation
- Fine needle aspiration (FNA): quick, good for cytology
- Core needle biopsy: better for architectural detail
- Excisional biopsy: gold standard for lymphoma but less common in carcinoma
Histology confirms:
Metastatic carcinoma vs lymphoma- Type and origin of the primary (via immunohistochemistry)
Management Principles in Nodal Metastatic Disease
Depends on primary tumour and extent of spread
Options include:
Surgical node clearance (e.g. axillary dissection)
Radiotherapy to involved fields
Systemic chemotherapy or targeted agents
In advanced cancers, nodal involvement may shift management to palliative intent
Prognostic Implications of Nodal Involvement
Nodal metastases worsen prognosis in nearly all solid tumours
Associated with:
Shorter survival
Higher recurrence risk
Upstaging in TNM classification
Nodal status often determines:
Adjuvant treatment need
Eligibility for curative surgery