Chronic Obstructive Pulmonary Disease (COPD)
content of this page
1- Introduction
2- Physiological Overview
3- Symptoms
4- Treatment
Introduction

Physiological Overview
Chronic Obstructive Pulmonary Disease (COPD) is a progressive lung disease characterized by persistent airflow limitation that is not fully reversible. The main physiological changes in COPD include:
1. Airway Inflammation and Structural Changes
- Chronic Inflammation: Similar to asthma, COPD involves ongoing inflammation in the airways and lung tissue. This inflammation is primarily driven by exposure to irritants, especially cigarette smoke.
- Airway Remodeling: Over time, the inflammation leads to structural changes in the airways, including thickening of the airway walls and increased mucus production.
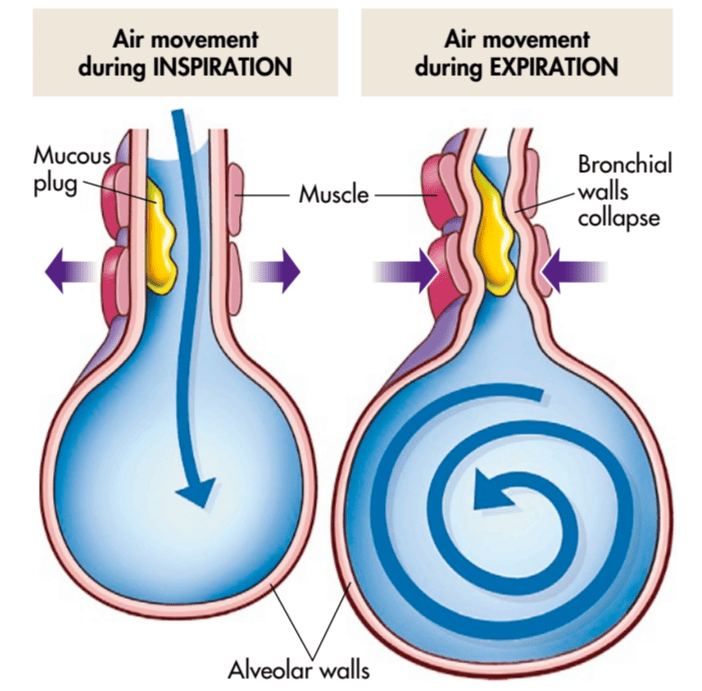
- Loss of Elasticity: Destruction of the lung tissue (emphysema) leads to loss of elasticity in the small airways and alveoli (air sacs), reducing the ability of the lungs to recoil during exhalation.
2. Bronchospasm and Airway Narrowing
- Bronchospasm: Episodes of bronchoconstriction can occur in COPD, particularly during exacerbations. This contributes to further narrowing of the airways and airflow limitation.
- Mucus Hypersecretion: Increased production of mucus by goblet cells in the airways contributes to airway obstruction and chronic cough.
3. Alveolar Destruction and Gas Exchange Impairment
- Emphysema: Destruction of the alveolar walls reduces the surface area available for gas exchange, leading to impaired oxygenation and carbon dioxide elimination.
- Loss of Lung Parenchyma: The destruction of lung parenchyma (emphysema) contributes to the irreversible airflow limitation seen in COPD.
4. Pulmonary Vascular Changes
- Pulmonary Hypertension: Chronic hypoxia (low oxygen levels) in COPD can lead to pulmonary hypertension, which further strains the right side of the heart.
- Cor Pulmonale: In severe cases, chronic pulmonary hypertension can cause right ventricular hypertrophy and eventually heart failure, known as cor pulmonale.
Symptoms and Clinical Manifestations
- Chronic Cough: Persistent cough with or without sputum production.
- Dyspnea: Gradually worsening shortness of breath, especially during physical exertion.
- Wheezing: Due to airflow limitation and bronchospasm.
- Chest Tightness: Feeling of pressure or discomfort in the chest.
- Frequent Respiratory Infections: Due to impaired clearance of mucus and weakened immune response.
Diagnosis and Management
- Spirometry: Key diagnostic test to confirm airflow limitation (FEV1/FVC ratio < 0.70).
- Imaging: Chest X-ray or CT scan to assess lung structure and rule out other conditions.
- Smoking Cessation: Critical for slowing disease progression.
- Medications: Bronchodilators (beta-agonists, anticholinergics) and inhaled corticosteroids to improve symptoms and reduce exacerbations.
- Pulmonary Rehabilitation: Exercise training, education, and behavioral interventions to improve quality of life.
- Oxygen Therapy: Supplemental oxygen for patients with severe hypoxemia.
- Surgery: Lung volume reduction surgery or lung transplantation for selected patients with severe emphysema.
Prognosis
- Progressive Disease: COPD is a progressive disease with variable rates of progression depending on individual factors such as smoking history, genetics, and exposure to pollutants.
- Exacerbations: Acute exacerbations can lead to further decline in lung function and increased mortality.
Symptoms
Chronic Obstructive Pulmonary Disease (COPD) manifests with a range of symptoms that can vary in severity and progression. The main symptoms include:
Chronic Cough: Persistent cough that may produce mucus (sputum). The cough is often worse in the morning and can be a daily occurrence.
Dyspnea (Shortness of Breath):
- Initially occurs during physical exertion (like climbing stairs or walking uphill).
- Progresses to occur during daily activities and eventually even at rest in severe cases.
Wheezing: A high-pitched or whistling sound when breathing, especially during exhalation. It is caused by narrowed airways and airflow limitation.
Chest Tightness: A feeling of pressure or heaviness in the chest, often associated with difficulty breathing.
Sputum Production: Increased production of mucus (sputum) from the lungs, which can be clear, white, yellow, or greenish in color.
Fatigue: Feeling tired or lacking energy, which can be related to the increased effort required to breathe.
Weight Loss: Particularly in advanced stages of COPD, due to increased energy expenditure and reduced appetite.
Frequent Respiratory Infections: COPD makes individuals more susceptible to respiratory infections, leading to episodes of exacerbations (acute worsening of symptoms).
These symptoms can vary in intensity and may fluctuate over time, especially with exacerbations triggered by infections or environmental factors.
Advanced Symptoms (Severe COPD):
- Cyanosis: Bluish discoloration of the lips or fingernail beds due to low oxygen levels in the blood.
- Edema: Swelling in the ankles or legs, often due to complications such as heart failure (cor pulmonale) secondary to COPD.
- Barrel Chest: In advanced emphysema, the chest may appear larger and barrel-shaped due to hyperinflation of the lungs.
Treatment
The treatment of Chronic Obstructive Pulmonary Disease (COPD) aims to alleviate symptoms, improve quality of life, and reduce the frequency and severity of exacerbations. Treatment strategies typically involve a combination of medications, lifestyle modifications, pulmonary rehabilitation, and sometimes surgical interventions. Here’s an overview of the main components of COPD treatment:
1. Medications
a. Bronchodilators
- Short-Acting Bronchodilators: Used for quick relief of symptoms during exacerbations. Examples include short-acting beta-agonists (SABA) like albuterol and short-acting anticholinergics like ipratropium.
- Long-Acting Bronchodilators: Provide sustained bronchodilation and are used as maintenance therapy. Examples include long-acting beta-agonists (LABA) and long-acting anticholinergics (LAMA). They can be prescribed alone or in combination with each other or with inhaled corticosteroids.
b. Inhaled Corticosteroids (ICS)
- Used in combination with LABA or LAMA in patients with more severe COPD and frequent exacerbations, or when there is significant eosinophilic inflammation.
- Help reduce airway inflammation and prevent exacerbations.
c. Phosphodiesterase-4 Inhibitors
- Medications like roflumilast may be used in patients with severe COPD and chronic bronchitis who have frequent exacerbations despite other treatments. They reduce inflammation and improve lung function.
2. Oxygen Therapy
- Long-term Oxygen Therapy (LTOT): Recommended for patients with severe COPD and chronic hypoxemia to improve survival and reduce symptoms.
- Ambulatory Oxygen Therapy: Provides supplemental oxygen during exercise and other activities to relieve breathlessness.
3. Pulmonary Rehabilitation
- Exercise Training: Designed to improve exercise capacity and muscle strength, reduce dyspnea, and enhance overall quality of life.
- Education: Includes teaching about COPD, medications, breathing techniques, and self-management strategies.
- Nutritional Counseling: Helps optimize nutritional status, which can be affected by COPD symptoms and medications.
4. Smoking Cessation
- Quitting smoking is crucial to slow disease progression and improve symptoms. Supportive therapies and counseling are available to help individuals quit.
5. Vaccinations
- Annual Influenza Vaccine: Reduces the risk of influenza-related complications.
- Pneumococcal Vaccine: Protects against pneumococcal infections, which can cause pneumonia and exacerbations in COPD patients.
6. Surgical Interventions
- Lung Volume Reduction Surgery (LVRS): Removes damaged lung tissue to improve lung function and quality of life in selected patients with severe emphysema.
- Lung Transplantation: Considered for patients with end-stage COPD who have severe symptoms despite optimal medical therapy.
7. Management of Exacerbations
- Prompt Treatment: Includes bronchodilators, corticosteroids, antibiotics (if bacterial infection is suspected), and oxygen therapy as needed.
- Preventive Strategies: Education on recognizing early symptoms of exacerbations and action plans to manage them promptly.
8. Supportive Care
- Psychological Support: COPD can affect mental health due to chronic symptoms and limitations in daily activities.
- End-of-Life Care Planning: For patients with advanced COPD, discussions about goals of care, advance directives, and palliative care options.