Cystic Fibrosis (CF)
content of this page
1- Introduction
2- Physiological Overview
3- Symptoms
4- Treatment
Introduction
CF affects primarily whites (approximately 1 in 3200) and is one of the most common lethal genetic diseases in this ethnic group.
Physiological Overview
On a simplistic level, CF is characterized by abnormal secretions that cause obstructive
problems within the respiratory, digestive, and reproductive tracts. However, research suggests that there may be additional CF-associated primary defects, such as an intrinsic
proinflammatory state and abnormal local immune defenses in the lungs. The CF gene (CFTR) has been located on chromosome 7. Its mutation results in the abnormal expression of cystic fibrosis transmembrane conductance regulator (CFTR) protein, which is a cyclic adenosine monophosphate
(cAMP)–activated chloride channel present on the surface of many types of epithelial cells, including those lining airways, bile ducts, pancreas, sweat ducts, and vas deferens. Despite knowing that chloride transport is a fundamental abnormality, the exact disease mechanisms in CF have still not
been clearly defined at the cellular and end-organ levels.
Symptoms
Respiratory Symptoms:
- Persistent Cough: Often with thick, sticky mucus that may be difficult to clear.
- Wheezing: High-pitched whistling sound when breathing, especially during exertion.
- Shortness of Breath: Especially during physical activity or when the airways are narrowed by mucus.
- Frequent Lung Infections: Due to the buildup of mucus that provides a breeding ground for bacteria.
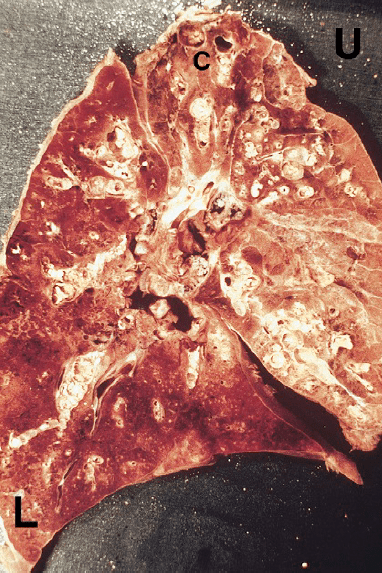
- Bronchiectasis: Permanent dilation of the bronchi (airways), which can worsen over time.
Digestive Symptoms:
- Pancreatic Insufficiency: Inability of the pancreas to produce sufficient enzymes for digestion, leading to:
- Steatorrhea: Foul-smelling, greasy stools.
- Malnutrition: Difficulty absorbing nutrients, especially fat-soluble vitamins (A, D, E, K).
- Intestinal Obstruction: Particularly in newborns (meconium ileus) or older children/adults (distal intestinal obstruction syndrome).
- Pancreatic Insufficiency: Inability of the pancreas to produce sufficient enzymes for digestion, leading to:
Other Symptoms:
- Salty-Tasting Skin: Due to the high concentration of salt in sweat.
- Dehydration: Because individuals with CF lose more salt in their sweat, they are prone to dehydration, especially during hot weather or exercise.
- Delayed Growth: CF can affect growth and development in children due to poor nutrient absorption and chronic illness.
Complications:
- Sinus Problems: Chronic sinusitis and nasal polyps are common.
- Diabetes: CF-related diabetes can develop due to damage to the pancreas.
- Osteoporosis: Reduced bone density due to malabsorption of vitamin D and poor nutritional status.
- Liver Disease: Cirrhosis or other liver complications may develop, especially in individuals with pancreatic insufficiency.
Treatment
Respiratory Management
Airway Clearance Techniques:
- Chest Physiotherapy: Techniques such as percussion and vibration to help loosen and clear mucus from the airways.
- Positive Expiratory Pressure (PEP) Therapy: Using a device that creates resistance during expiration to enhance mucus clearance.
- Flutter Valve: A handheld device that uses oscillations to mobilize mucus in the airways.
Inhaled Medications:
- Bronchodilators: To open the airways and improve airflow (e.g., albuterol).
- Mucolytics: Medications to thin mucus, making it easier to cough up (e.g., dornase alfa).
Antibiotics:
- Prophylactic Antibiotics: Regular use to prevent or manage chronic lung infections.
- IV Antibiotics: Intermittent courses to treat acute exacerbations of respiratory infections.
Lung Transplantation:
- Considered for individuals with advanced lung disease that does not respond to other treatments.
Nutritional Support
Pancreatic Enzyme Replacement Therapy (PERT):
- Pancreatic Enzymes: Taken with meals and snacks to help digest food and absorb nutrients.
High-Calorie Diet:
- Rich in protein and fat to meet increased energy needs due to malabsorption.
Fat-Soluble Vitamin Supplements:
- Vitamin A, D, E, and K supplements to compensate for malabsorption.
Nutritional Counseling:
- Guidance from dietitians to ensure adequate nutrition and monitor growth and development, especially in children.