Pneumonia
content of this page
1- Introduction
2- Physiological Overview
3- Symptoms
4- Treatment
Introduction
Physiological Overview
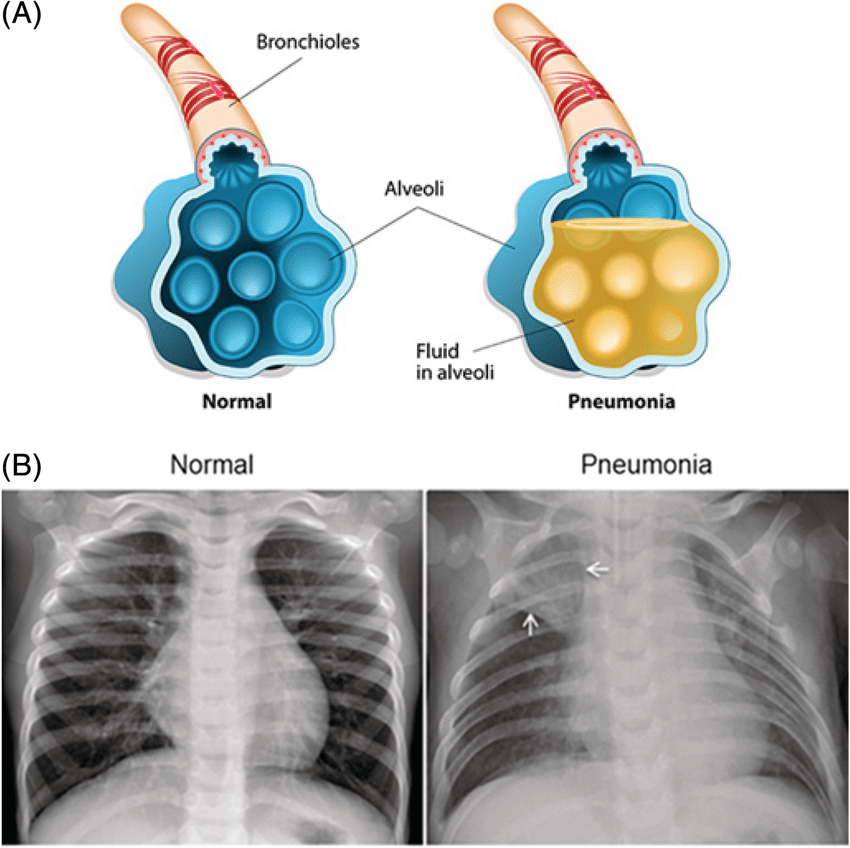
Pneumonia is an infection that inflames the air sacs in one or both lungs, causing them to fill with fluid or pus. This can make breathing painful and limit oxygen intake. Here’s a physiological overview of pneumonia:
1. Pathophysiology
- Infection: Pneumonia is usually caused by bacteria, viruses, fungi, or, less commonly, by other microorganisms.
- Inflammatory Response: The infection triggers an inflammatory response in the lungs, leading to the accumulation of fluid and cellular debris in the alveoli (air sacs).
- Consolidation: As the infection progresses, the affected lung tissue may become consolidated, making it less able to exchange oxygen and carbon dioxide effectively.
2. Types of Pneumonia
- Community-Acquired Pneumonia (CAP): Occurs outside of hospitals or healthcare settings, often caused by bacteria such as Streptococcus pneumoniae or viruses like influenza.
- Hospital-Acquired Pneumonia (HAP): Develops during a hospital stay and can be caused by bacteria that are more resistant to antibiotics.
- Ventilator-Associated Pneumonia (VAP): A type of HAP that occurs in people who are on ventilators in hospitals or other healthcare facilities.
3. Symptoms
- Cough: Often produces mucus, which may be green, yellow, or bloody.
- Fever: High fever with chills is common, especially in bacterial pneumonia.
- Difficulty Breathing: Shortness of breath, rapid breathing, and chest pain when breathing or coughing.
- Fatigue: Feeling very tired or weak.
- Confusion: Especially in older adults or those with severe pneumonia.
- Nausea and Vomiting: Particularly in children.
4. Diagnosis
- Physical Examination: Stethoscope to listen for crackling or bubbling sounds in the lungs (rales or crepitations).
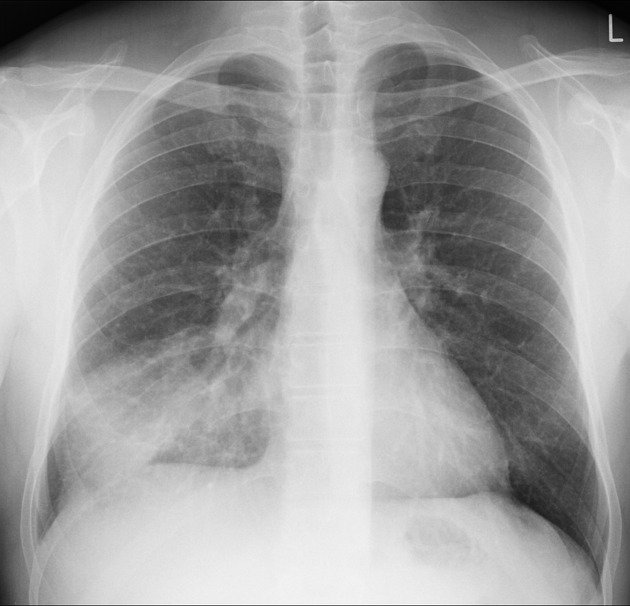
- Chest X-ray: To visualize the lungs and detect areas of inflammation or consolidation.
- Blood Tests: To identify the causative organism and assess the severity of infection (e.g., white blood cell count, C-reactive protein).
5. Treatment
- Antibiotics: Prescribed based on the likely causative organism (bacterial pneumonia) and its susceptibility to specific antibiotics.
- Antiviral or Antifungal Medications: Used for viral or fungal pneumonia, respectively.
- Supportive Care: Rest, fluids, and over-the-counter medications to relieve pain and fever.
- Oxygen Therapy: If blood oxygen levels are low.
- Hospitalization: For severe cases requiring intravenous antibiotics or intensive monitoring.
6. Complications
- Respiratory Failure: Severe pneumonia can lead to respiratory failure, where the lungs cannot provide enough oxygen or remove enough carbon dioxide from the blood.
- Sepsis: Infection spreads to the bloodstream, causing widespread inflammation and organ failure.
- Lung Abscess: Collection of pus within the lung tissue.
- Pleural Effusion: Build-up of fluid between the layers of tissue lining the lungs and chest cavity.
7. Prevention
- Vaccination: Annual influenza vaccine and pneumococcal vaccine to prevent certain types of bacterial pneumonia.
- Hand Hygiene: Regular handwashing to reduce the spread of respiratory infections.
- Smoking Cessation: Avoiding smoking and secondhand smoke to reduce the risk of pneumonia.
Symptoms
Pneumonia presents a variety of symptoms that can range from mild to severe, depending on the causative organism, the overall health of the individual, and other factors. Common symptoms of pneumonia include:
Cough: Often starts as a dry cough but can later produce phlegm (sputum) that may be green, yellow, or bloody.
Fever: High fever is common, especially in bacterial pneumonia. It may be accompanied by sweating and chills.
Shortness of Breath: Difficulty breathing or rapid breathing, which may be more pronounced with physical exertion.
Chest Pain: Sharp or stabbing chest pain that worsens with coughing or deep breathing. It may be localized or spread across the chest.
Fatigue: Feeling unusually tired or weak, which can interfere with daily activities.
Weakness: Generalized weakness or feeling lethargic.
Loss of Appetite: Reduced desire to eat or drink.
Confusion: Particularly in older adults or individuals with severe pneumonia.
Nausea and Vomiting: Especially in children.
Headache: Mild to severe headaches may occur, often associated with the fever and body aches.
Muscle Aches: Aching muscles, similar to those experienced with influenza.
Bluish Skin: In severe cases, lips or nails may have a bluish tint due to lack of oxygen.
Treatment
Treatment of pneumonia depends on several factors including the type of pneumonia (community-acquired, hospital-acquired, or aspiration), the severity of symptoms, and the overall health of the patient. Here’s an overview of the main components of pneumonia treatment:
1. Antibiotics
Bacterial Pneumonia: Antibiotics are the mainstay of treatment for bacterial pneumonia. The choice of antibiotic depends on the suspected or identified causative bacteria and its susceptibility to specific antibiotics. Commonly used antibiotics include:
- Macrolides: Such as azithromycin, clarithromycin.
- Fluoroquinolones: Such as levofloxacin, moxifloxacin.
- Cephalosporins: Like ceftriaxone, cefuroxime.
- Penicillins: Including amoxicillin or amoxicillin-clavulanate.
Viral Pneumonia: Antiviral medications may be used for pneumonia caused by influenza viruses or other specific viral pathogens. However, most cases of viral pneumonia are managed with supportive care.
Fungal Pneumonia: Antifungal medications, such as fluconazole or voriconazole, are used for pneumonia caused by fungi like Candida or Aspergillus.
2. Supportive Care
- Rest and Fluids: Adequate rest and increased fluid intake help the body recover and maintain hydration.
- Fever and Pain Relief: Over-the-counter medications like acetaminophen (paracetamol) or ibuprofen can reduce fever and alleviate pain.
- Oxygen Therapy: If oxygen levels are low, supplemental oxygen may be provided.
- Cough Management: Medications may be prescribed to help control cough and loosen mucus.
3. Hospitalization
- Severe Cases: Patients with severe pneumonia, especially those with underlying health conditions or complications, may require hospitalization.
- Intravenous Antibiotics: Administered in the hospital to ensure effective delivery and monitoring of treatment.
- Monitoring: Regular monitoring of vital signs, oxygen levels, and response to treatment.
4. Prevention of Complications
- Respiratory Support: Mechanical ventilation or non-invasive ventilation may be necessary for patients with severe respiratory distress or respiratory failure.
- Fluid Management: Ensuring adequate fluid intake while monitoring for signs of dehydration.
- Nutritional Support: Especially important for patients who have difficulty eating due to illness.
5. Vaccination
- Influenza Vaccine: Annual vaccination to prevent pneumonia caused by influenza viruses.
- Pneumococcal Vaccine: Recommended for adults over 65, children, and individuals with certain medical conditions to protect against Streptococcus pneumoniae, a common cause of bacterial pneumonia.
6. Follow-Up Care
- Monitoring: Regular follow-up visits to assess recovery, check lung function, and ensure complete resolution of symptoms.
- Rehabilitation: Pulmonary rehabilitation may be recommended to improve lung function and overall physical condition, especially in severe cases.
7. Lifestyle Modifications
- Smoking Cessation: Quitting smoking and avoiding exposure to secondhand smoke to reduce the risk of pneumonia and other respiratory illnesses.
- Hand Hygiene: Regular handwashing to prevent the spread of respiratory infections.