Pulmonary Fibrosis
Content of This Page
1- Introduction
2- Causes
3- Symptoms
4- Stages of The Disease
5- Treatment
6- What Should You Avoid
Introduction
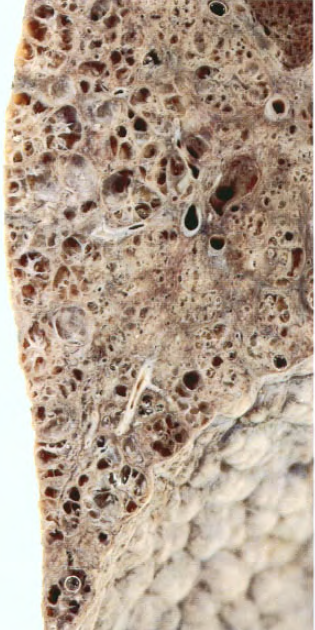
Pulmonary Fibrosis is a lung disease characterized by the formation of scar tissue (fibrosis) in the lungs. This scarring leads to a progressive decline in lung function, making it difficult to breathe deeply and efficiently. The disease can result from various causes, including environmental exposures, certain medications, or autoimmune conditions, and often leads to symptoms such as persistent cough, shortness of breath, and fatigue.
Causes
- Idiopathic: No known cause, often referred to as idiopathic pulmonary fibrosis (IPF).
- Environmental Exposures: Long-term exposure to pollutants, dust, or toxic fumes.
- Medications: Certain drugs, such as chemotherapy agents or antibiotics.
- Autoimmune Diseases: Conditions like rheumatoid arthritis, systemic sclerosis, or lupus.
- Genetics: Family history and genetic mutations can increase risk.
- Infections: Past viral infections or chronic lung infections.
- Radiation Therapy: Treatment for cancers that can lead to lung scarring.
Symptoms
- Persistent dry cough
- Shortness of breath, especially with exertion
- Fatigue
- Unexplained weight loss
- Clubbing of the fingers or toes (widening and rounding)
- Chest discomfort or pain

Stages of The Disease
Early Stage:
- Symptoms are mild and may include a persistent cough and slight breathlessness, often not severe enough to significantly impact daily activities.
Intermediate Stage:
- Symptoms become more noticeable, with increased shortness of breath, fatigue, and a persistent cough. Daily activities may start to be affected.
Advanced Stage:
- Severe breathlessness, significant impact on daily life, and possibly complications such as respiratory failure or heart issues. Quality of life is notably affected.
End-Stage:
- Severe lung damage with major functional impairment, requiring supplemental oxygen or advanced interventions. Overall prognosis is poor without a lung transplant.
Treatment
Medications:
- Antifibrotics: To slow disease progression (e.g., pirfenidone, nintedanib).
- Corticosteroids: To reduce inflammation (used cautiously due to potential side effects).
Oxygen Therapy:
- To improve oxygen levels in the blood and relieve symptoms of shortness of breath.
Pulmonary Rehabilitation:
- A program that includes exercise, education, and support to help manage symptoms and improve quality of life.
Lung Transplant:
- Considered for advanced cases where other treatments are ineffective.
Lifestyle Changes:
- Quit Smoking: If applicable.
- Healthy Diet: To support overall health and manage symptoms.
- Avoid Environmental Irritants: Such as dust or fumes.
Supportive Care:
- Includes managing symptoms and complications, such as infections or heart issues.
What Should You Avoid
- Smoking
- Exposure to environmental pollutants
- Excessive alcohol consumption
- Inhaling dust or fumes
- Certain medications (as advised by a doctor)
- Inactivity or lack of exercise