Glomerulonephritis
content of this page
1- Introduction
2- Pathophysiology
3- Symptoms
4- Treatment
Introduction
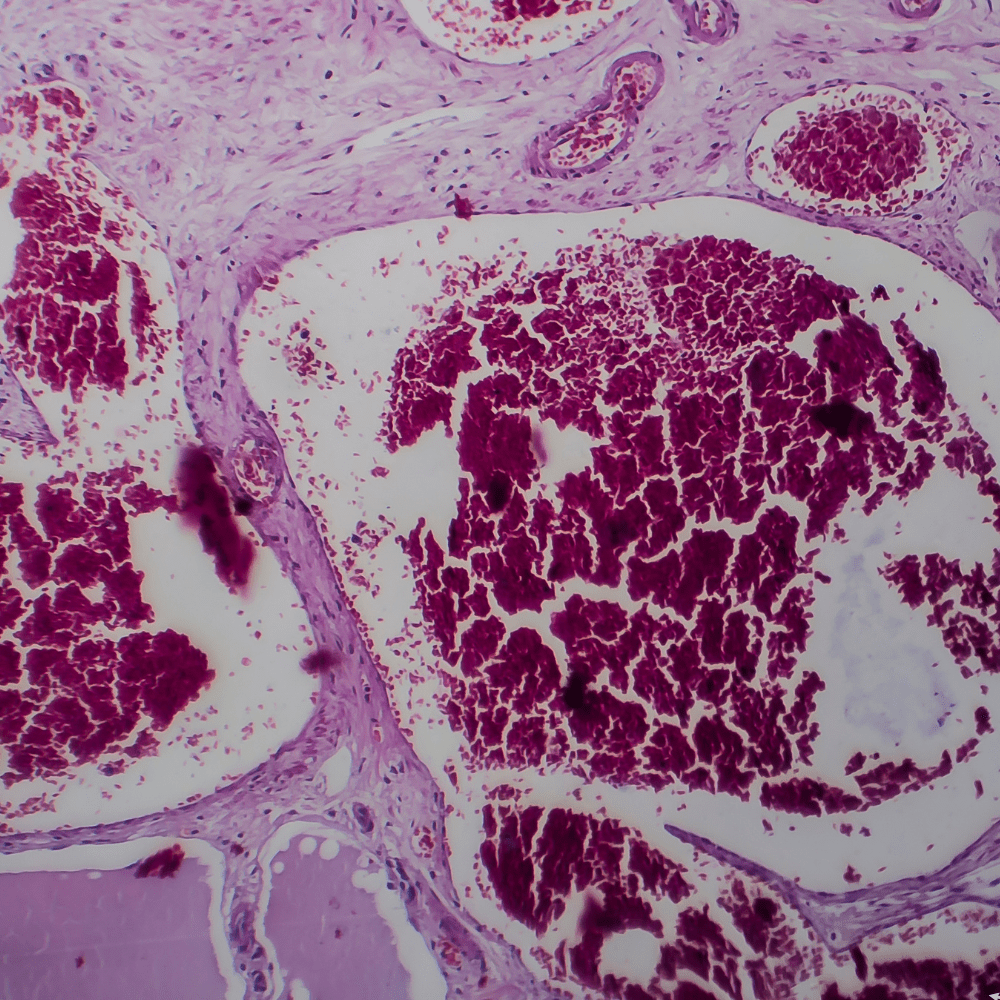
Glomerulonephritis is an inflammation of the glomerulus caused by numerous factors, including infection, immunologic abnormalities (the most common cause), ischemia, free radicals, drugs, toxins, vascular disorders, and systemic diseases, including diabetes mellitus and lupus erythematosus. Glomerular disease is the most common cause of chronic kidney disease and end-stage renal failure. The classification of glomerulonephritis can be described according to cause, pathologic lesions, disease progression (acute, rapidly progressive, chronic), or clinical presentation (nephrotic syndrome, nephritic syndrome, acute or chronic kidney failure).
Pathophysiology
Glomerulonephritis refers to a group of kidney diseases characterized by inflammation and damage to the glomeruli, which are the tiny filtering units in the kidneys responsible for removing waste products and excess fluids from the blood. The pathophysiology of glomerulonephritis involves complex immune-mediated processes, structural changes in the glomeruli, and subsequent impairment of kidney function. Here’s an overview of the key pathophysiological mechanisms:
Immune-Mediated Injury:
- Many forms of glomerulonephritis are immune-mediated, meaning they involve abnormal immune responses that lead to inflammation and damage within the glomeruli.
- Immune Complex Deposition: Antigen-antibody complexes or other immune complexes can deposit in the glomerular basement membrane (GBM) or mesangium (the supportive tissue between glomerular capillaries), triggering an inflammatory response.
- Autoimmune Reactions: In some types of glomerulonephritis, such as IgA nephropathy or lupus nephritis, the immune system mistakenly attacks the glomeruli or deposits immune complexes in them, leading to inflammation and injury.
Complement Activation:
- Activation of the complement system, a part of the immune system involved in inflammation and immune response, plays a critical role in the pathogenesis of glomerulonephritis.
- Alternative Pathway Activation: Dysregulation of the alternative complement pathway can contribute to glomerular injury in diseases like membranoproliferative glomerulonephritis (MPGN).
Endothelial Cell Injury:
- Inflammation within the glomeruli can lead to injury and dysfunction of endothelial cells lining the glomerular capillaries.
- Increased Permeability: Damage to endothelial cells can increase the permeability of the glomerular capillaries, allowing proteins (such as albumin) to leak into the urine (proteinuria).
Mesangial Cell Proliferation:
- Mesangial cells, located in the mesangium of the glomerulus, play a role in supporting the glomerular structure and regulating blood flow within the glomerular capillaries.
- In response to immune complex deposition and inflammation, mesangial cells may proliferate (increase in number) and produce matrix proteins, contributing to glomerular scarring and impaired filtration function.
Glomerular Basement Membrane (GBM) Alterations:
- The GBM, a specialized structure that separates the blood in the glomerular capillaries from the urine in the urinary space, can become thickened or damaged in glomerulonephritis.
- Increased Permeability: Changes in the GBM can lead to increased permeability to proteins and other substances, contributing to proteinuria.
- Scarring (Glomerulosclerosis): Chronic inflammation and injury can lead to glomerular scarring (glomerulosclerosis), which impairs kidney function over time.
Clinical Manifestations:
- The pathophysiological changes in glomerulonephritis result in clinical manifestations such as:
- Proteinuria: Protein (especially albumin) leaking into the urine due to increased glomerular permeability.
- Hematuria: Blood in the urine due to damage to the glomerular capillaries.
- Edema: Fluid retention due to decreased kidney function and loss of protein in the urine.
- Hypertension: Increased blood pressure due to fluid retention and activation of the renin-angiotensin-aldosterone system.
- The pathophysiological changes in glomerulonephritis result in clinical manifestations such as:

Symptoms
Glomerulonephritis (GN) encompasses a range of kidney conditions characterized by inflammation of the glomeruli, which are the filtering units of the kidneys responsible for removing waste and excess fluids from the blood. The symptoms of glomerulonephritis can vary depending on the underlying cause, the extent of kidney damage, and whether the condition is acute or chronic. Here are the common symptoms associated with glomerulonephritis:
Hematuria:
- One of the hallmark symptoms of glomerulonephritis is the presence of blood in the urine (hematuria). The urine may appear pink, red, or cola-colored due to the leakage of red blood cells from the damaged glomeruli into the urine.
Proteinuria:
- Glomerulonephritis often leads to the leakage of proteins, particularly albumin, from the blood into the urine (proteinuria). This can result in frothy or foamy urine.
Edema:
- Swelling (edema) may occur, typically around the eyes, hands, feet, ankles, and abdomen. Edema results from the loss of proteins (like albumin) into the urine, leading to fluid retention.
Hypertension:
- Elevated blood pressure (hypertension) is common in glomerulonephritis. Kidney damage can lead to the activation of the renin-angiotensin-aldosterone system, which regulates blood pressure, and fluid retention can further contribute to hypertension.
Decreased Urine Output:
- In severe cases or acute exacerbations, glomerulonephritis can lead to reduced urine output (oliguria) or even complete cessation of urine production (anuria).
Fatigue and Weakness:
- Reduced kidney function can lead to anemia (due to decreased production of erythropoietin) and buildup of waste products in the blood, causing fatigue, weakness, and malaise.
Foamy Urine:
- Due to proteinuria, urine may appear foamy or bubbly, especially noticeable during urination.
Puffiness Around Eyes:
- Edema can cause puffiness or swelling around the eyes, known as periorbital edema.
Joint Pain:
- Some forms of glomerulonephritis, such as IgA nephropathy (also known as Berger’s disease), may be associated with joint pain and swelling.
Abdominal Pain:
- Pain in the abdomen may occur due to fluid accumulation (ascites) or inflammation of the kidneys.
Nausea and Vomiting:
- Accumulation of waste products and electrolyte imbalances can lead to gastrointestinal symptoms such as nausea and vomiting.
Fever:
- In cases where glomerulonephritis is secondary to an infection or autoimmune condition, fever may be present.
Treatment
The treatment of glomerulonephritis (GN) aims to manage symptoms, slow down disease progression, and preserve kidney function. The approach to treatment depends on the underlying cause of GN, the severity of kidney damage, and whether the condition is acute or chronic. Here’s an overview of the treatment strategies commonly used for glomerulonephritis:
Identification and Management of Underlying Cause:
- Infections: If glomerulonephritis is caused by a bacterial or viral infection (such as streptococcal infection), antibiotics or antiviral medications may be prescribed.
- Autoimmune Disorders: In autoimmune forms of GN (such as lupus nephritis or IgA nephropathy), immunosuppressive medications (such as corticosteroids, cyclophosphamide, or mycophenolate) may be used to suppress the immune response and reduce inflammation.
- Systemic Diseases: Treatment focuses on managing the underlying systemic disease (e.g., diabetes, hypertension) to prevent further kidney damage.
- Genetic Conditions: Genetic forms of GN may require specialized genetic counseling and management.
Control of Blood Pressure:
- Controlling hypertension is crucial in managing glomerulonephritis. Medications such as angiotensin-converting enzyme (ACE) inhibitors or angiotensin II receptor blockers (ARBs) are commonly used to lower blood pressure and reduce proteinuria, thereby slowing the progression of kidney disease.
Reduction of Proteinuria:
- Medications that reduce proteinuria (such as ACE inhibitors or ARBs) are beneficial in preserving kidney function and reducing the risk of complications associated with protein loss.
Diuretics:
- Diuretics may be prescribed to help reduce edema (swelling) and manage fluid retention, especially in cases where there is significant fluid overload.
Management of Fluid and Electrolyte Balance:
- Monitoring and correcting electrolyte imbalances (such as potassium or sodium levels) are important in preventing complications associated with electrolyte disturbances.
Dietary Modifications:
- Depending on the type and stage of GN, dietary changes may be recommended to manage symptoms and support kidney function. This may include reducing protein intake to reduce the workload on the kidneys and managing fluid and electrolyte intake.
Regular Monitoring and Follow-up:
- Regular monitoring of kidney function through blood tests (such as serum creatinine, estimated glomerular filtration rate) and urine tests (such as urine albumin-to-creatinine ratio) is essential to assess disease progression and adjust treatment accordingly.
- Monitoring for complications such as hypertension, anemia, and bone disease (renal osteodystrophy) is also important.
Symptomatic Treatment:
- Symptomatic relief may include medications for pain management, management of nausea and vomiting, and addressing other symptoms associated with GN and its treatment.
Renal Replacement Therapy:
- In advanced stages of chronic glomerulonephritis or in cases of end-stage renal disease (ESRD), renal replacement therapy such as dialysis or kidney transplantation may be necessary.
Lifestyle Modifications:
- Lifestyle changes such as smoking cessation, maintaining a healthy weight, regular exercise, and avoiding nephrotoxic substances are important in managing and preventing further kidney damage.